PAD is a lifelong medical condition. Once you have been diagnosed with PAD, you will need to regularly see a doctor who specializes in vascular (blood vessel) diseases. You will need to take steps to prevent complications. Learn the warning signs of a medical emergency related to PAD, below.
A team of healthcare professionals can help you manage PAD and treat any complications. You may need to see specialists in vascular (blood vessel) medicine, cardiologists to treat heart disease, radiologists to do imaging tests, vascular surgeons to perform procedures to improve blood flow, infectious disease specialists to treat infections, physical therapists to guide your exercise program, podiatrists to provide foot care, and nutritionists to help you plan healthy meals.
Manage your condition
It is important to get routine medical care and to take all medicines as your doctor prescribes.
- Talk with your doctor about how often you should schedule office visits and blood tests or other tests.
- Call your doctor between visits if you start to have leg pain that does not go away after a few minutes of rest or if any other PAD symptoms get worse. Changes in symptoms could be a sign of PAD complications.
- Get recommended vaccines, including the pneumococcus and influenza (flu) shots, every year at the start of flu season. Anyone who lives with you or whom you see often should also get regular vaccines.
Follow up with your doctor regularly to check your risk factors, monitor symptoms, and assess your legs and feet.
Take care of your feet
Foot problems are a common complication of PAD. If you develop a foot sore, you’ll need regular care to help the sore heal and prevent infection.
Many people who have PAD also have diabetes, which raises the risk of complications that may lead to amputation, a type of surgery to remove all or part of a foot or leg. Diabetes may also cause nerve problems that make it hard to sense when you have injured your feet.
You can reduce your risk for foot ulcers and infections by taking care of your feet.
- Always wear socks and shoes. Socks should not have any seams. Wear comfortable shoes that fit well and protect your feet. Your shoes should have low heels and shock-absorbing soles to reduce pressure on the bottom of your foot. Shoes should have fasteners to prevent rubbing. Your doctor may recommend that you visit a specialist who can modify your shoes to reduce your chance of getting sores on your feet.
- Check your feet every day for injuries or sores. If you have PAD and diabetes, have your doctor examine your feet twice a year.
- Do not go barefoot. This will help prevent foot injury that can lead to ulcers and infections, which are more likely when you have poor circulation.
- Follow your doctor’s instructions about caring for incisions (openings) made in the skin of your legs or feet during surgery or a procedure for treating PAD. Return to Treatment to review possible treatment options for PAD.
- See your doctor for any foot problems. Do not treat corns, calluses, long or ingrown nails, or other foot problems yourself to avoid injuries that could lead to sores or infections.
Women and PAD
Certain conditions during pregnancy, such as preeclampsia (a high-blood pressure disorder) or gestational diabetes (high blood sugar during pregnancy), can raise a woman’s risk of developing PAD later in life.
PAD affects women and men differently. Women’s PAD symptoms may be worse than men’s. Women who have PAD often cannot walk as far or as fast as men who have PAD. They also report lower quality of life than men, perhaps because it’s harder to walk and take part in daily activities. Depression is also more common in women who have PAD than in men who have PAD.
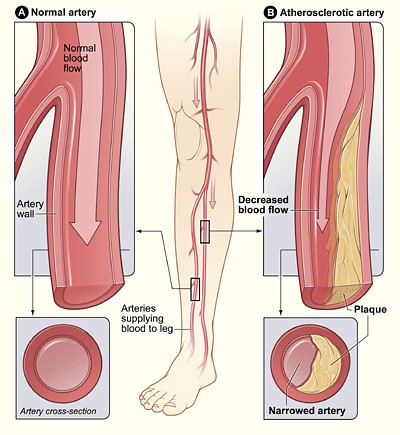
Diseases linked with PAD
People who have PAD have lifestyle habits and other factors, such as a family history, that make it more likely that they will develop other diseases related to atherosclerosis, including the following:
If you have PAD with symptoms, your doctor may use ultrasound to screen you for abdominal aortic aneurysm.
Control your blood pressure
If you have high blood pressure, it is important that you continue your treatment plan. Following your treatment plan, getting regular follow-up care, and learning how to monitor your condition at home are important. Let your doctor know if you are planning to become pregnant. These steps can help prevent or delay complications that high blood pressure can cause.
Your doctor may adjust your treatment plan as needed to lower or control your high blood pressure.
Follow your diabetes care plan
If you have diabetes, your doctor will recommend lifestyle changes, including a special eating plan, and may prescribe medicines to manage blood sugar levels. Managing diabetes carefully can lower your risk of complications.
Be alert for sores on your feet or legs, and call your doctor if you see signs of a sore getting infected, such as redness, swelling, pain, or pus, or if you have a fever or chills. To treat sores, your doctor may prescribe antibiotics, clean the sores, remove dead tissue with surgery and apply medicines and bandages to the area.
Manage your blood cholesterol levels
If you have unhealthy levels of blood cholesterol, it is important that you continue your treatment. Follow-up care depends on your cholesterol levels, your risk of complications such as a heart attack or a stroke, and your response to treatment.
Take care of your mental health
Living with PAD may cause fear, anxiety, depression, and stress. You may worry about having heart problems or making lifestyle changes that are necessary for your health. Some people become depressed because of problems with walking and daily activities. PAD might also lead to concerns about the risk of amputation.
By lowering stress levels and learning coping skills, you may be able to live longer and improve your quality of life. Talk with your healthcare team about how you feel. Your doctor may recommend you take steps such as these:
- Join a patient support group. This may help you adjust to living with PAD. You can find out how other people manage similar symptoms. Your doctor may be able to recommend local support groups, or you can check with an area medical center.
- Seek support from family and friends. Letting your loved ones know how you feel and what they can do to help you can help relieve stress and anxiety.
- Talk to a professional counselor. If you have depression or anxiety, your doctor may also recommend medicines or other treatments that can improve your quality of life.
Know when to call for help
PAD puts you at high risk of serious health problems. If you think that you are having symptoms of PAD, check with your doctor. For the following conditions, call 9-1-1 right away. Every minute matters.
Acute limb ischemia
Acute limb ischemia is a medical emergency that must be treated rapidly to avoid amputation or other serious problems. Seek medical help right away if:
- You cannot feel or move your foot
- Your leg or foot hurts or feels like “pins and needles” while resting
- One foot is paler or colder than the other
Bloodstream infection
When bacteria enter the blood from an infected sore, they can cause a bloodstream infection. Symptoms include fever and chills. Intravenous (IV) antibiotics need to be given right away in a hospital. If a blood infection is not treated in time, or if the immune system can’t control the infection, the body’s inflammatory response can lead to septic shock, organ failure, or even death.
Bone infections
If you develop deep ulcers over bones, you are at risk for a bone infection called osteomyelitis. Symptoms include bone pain; excessive sweating; fever and chills; swelling, redness, pain, and warmth at the site of infection; and an open wound that may show pus. Treatment includes antibiotics, surgery to remove infected bone, and procedures to improve blood flow. Treatment may have to be given in a hospital.
Cellulitis
Cellulitis is a skin infection that can spread to the deep tissues of the skin and muscle. Symptoms include areas of the skin that are warm, swollen, and tender. Cellulitis can also cause fever, chills, swollen lymph nodes, and blisters.
Your doctor may prescribe antibiotics to take by mouth. If the infection gets worse or if you get very sick, you may need to stay in the hospital for treatment.