Overview
Restoration of immune function is critical to the success of potential immunotherapies for glioblastoma (GBM). Tumor-derived mediators of immune suppression represent potentially druggable targets, and limiting their function may be sufficient to rescue immune function. In particular, our group is interested in targeting GBM EV-myeloid cell interactions, a critical therapeutic axis for inhibiting the formation of immunosuppressive myeloid cells. The multimodal signaling capabilities of EVs make them an appealing therapeutic target, as inhibiting their efficacy has the potential to attenuate multiple immunosuppressive pathways.
Areas of Concentration
Mechanisms of Tumor-Mediated Immune Suppression in Glioblastoma (GBM)
GBM is the most common and deadly intrinsic brain tumor in adults, for which novel therapies are urgently needed. Immunotherapy has revolutionized the treatment of some cancers in recent years, but efforts in GBM have thus far been discouraging. A critical barrier to the development of effective immunotherapy in GBM is the profound immune suppression exhibited by GBM patients. The pathophysiology of GBM-mediated immune suppression is poorly understood and multifactorial, and it includes modulation of the tumor microenvironment, induction of immunosuppressive myeloid cells, and the systemic release of immunosuppressive factors.
Tumor-Derived Extracellular Vesicles (EVs)
EVs are biologically complex molecules capable of carrying myriad signals to target cells, both locally and systemically. EVs carry both soluble and surface-bound proteins, as well as short, non-coding RNAs, including pi-RNAs and y-RNAs. EVs interact with target cells through similarly diverse mechanisms: surface interactions, endocytotic uptake, and direct membrane fusion. This diversity of tools enable EVs to recapitulate many of the interactions of a nucleated cell, underscoring a fundamental biologic role we are only beginning to understand.
Selected Publications
Himes BT, Peterson TE, Tyson J, Lee HJL, de Mooij T, Cumba Garcia LM, Jung M, Yan D, Uhm S, Abukhadra M, Parney DLN, Gustafson MP, Dietz AB, Johnson AJ, Dong H, Maus R, Markovic S, Lucien-Matteoni F, Parney IF. The Role of Extracellular Vesicles and PD-L1 in Glioblastoma-Mediated Immunosuppressive Monocyte Induction. Neuro-Oncology. 2020 Jul; 22(7), 967-978. PMID: 32080744
Himes BT, Lee HJL, Geiger PA, Fain CE, Tritz ZP, Peterson TE, Parney IF. Use of heparin to rescue immunosuppressive monocyte reprogramming by glioblastoma-derived extracellular vesicles. Journal of Neurosurgery. 2022 Sep; 1-11 (aop). PMID: 36115048
Himes BT, Geiger PA, Ayasoufi K, Bhargav AG, Brown DA, Parney IF. Immunosuppression in glioblastoma: current understanding and therapeutic implications. Frontiers in Oncology. 2021 Oct; 11:770561. PMID: 34778089
Ayasoufi K, Pfaller CK, Evgin L, Khadka RH, Tritz ZP, Goddery EN, Fain CE, Yokanovich LT, Himes BT, Jin F, Zheng J, Schuelke MR, Hansen MJ, Tung W, Parney IF, Pease LR, Vile RG, Johnson AJ. Brain cancer induces systemic immunosuppression through release of non-steroid soluble mediators. Brain. 2020 Dec; 143(12), 3629-3652 PMID: 33253355
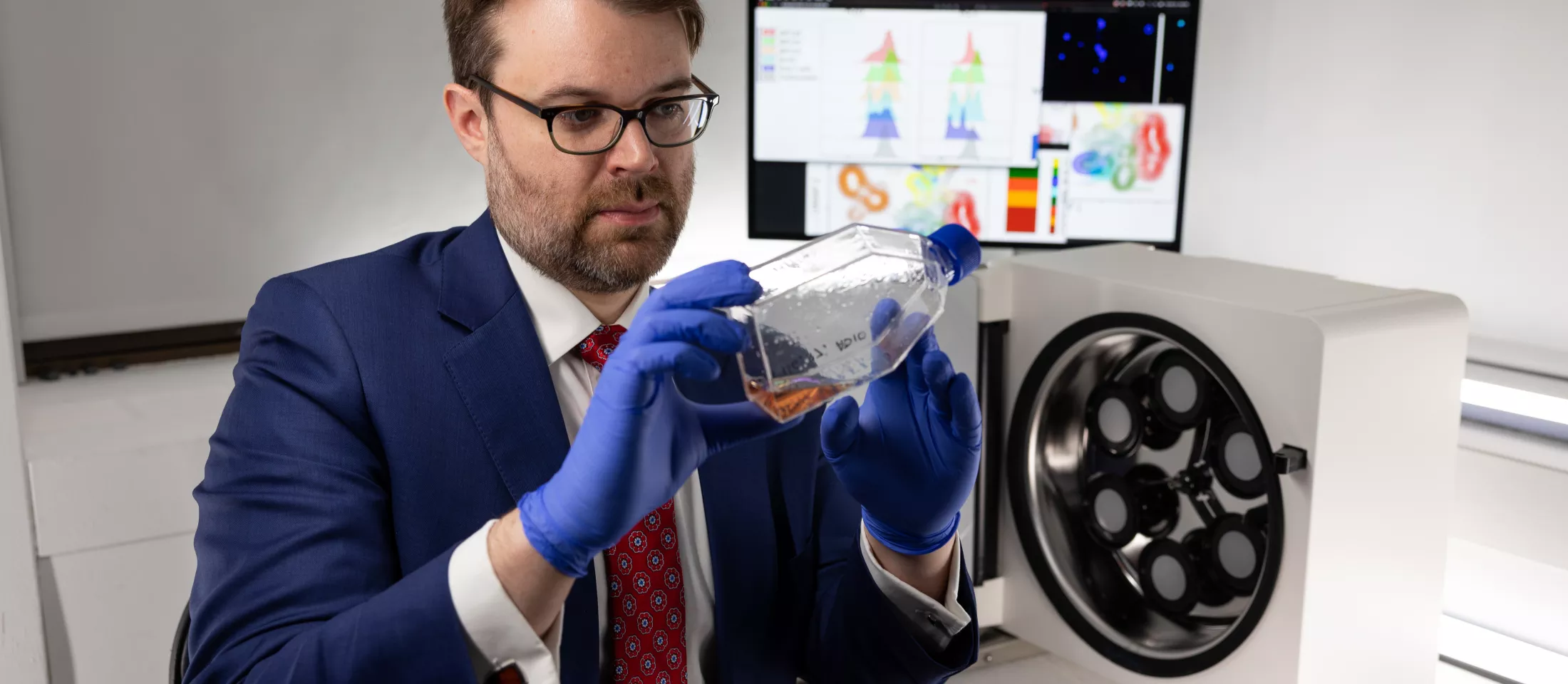
Benjamin T. Himes, MD, PhD
About Benjamin T. Himes MD, PhD, MHS
Dr. Himes received his Bachelor of Arts degree in biology with a concentration in neuroscience from the University of Pennsylvania. He earned his medical degree and a Master of Health Science from the Yale School of Medicine, where he also completed a Howard Hughes Fellowship. He subsequently pursued his neurosurgical residency training at the Mayo Clinic in Rochester, MN. During that time he completed a PhD in biomedical sciences (immunology track) under the mentorship of Ian F. Parney MD, PhD, and received the Andrew T. Parsa Research Fellowship Grant from the Neurosurgery Research and Education Foundation. Dr. Himes subsequently completed a fellowship in neurosurgical oncology, also at Mayo Clinic, prior to joining the faculty at Montefiore Einstein in 2022.