Atrial Fibrillation/Flutter
At the Montefiore Einstein Center for Heart and Vascular Care, you can access exceptional care for atrial fibrillation/flutter. As a global leader in cardiovascular medicine and surgery, we are an academic-based, national and international referral site for high-risk and complex cases. For more than a century, we have been at the forefront in treating heart disease.
Ranked in the top one percent of all hospitals in the nation for Cardiology, Heart & Vascular Surgery according to U.S. News & World Report, our specialists are passionate about uncovering the latest diagnostic approaches and treatments that can improve outcomes. Backed by a multidisciplinary team of specialists, Montefiore Einstein continues to make advances in the treatment of heart disease. In recent years, we have expanded our programs in advanced cardiac imaging, heart failure and interventional cardiovascular medicine and assembled a world-renowned cardiothoracic surgical team.
When you trust us with your care, you can expect compassionate, personalized treatment plans that meet the highest standards for quality and safety. In addition, we offer patients a full choice of support services, from nutritional guidance to rehabilitative therapies.
When you need care for atrial fibrillation/flutter, turn to our dedicated providers who will develop a highly personalized treatment plan specific to you.
As part of an academic health system, Montefiore Einstein Center for Heart and Vascular Care supports the mission and guidelines of the U.S. Department of Health and Human Services (HHS). The following information is provided by HHS.
Atrial Fibrillation Risk Factors
Age, family history and genetics, lifestyle, heart disease or other medical conditions, race, sex, and a history of surgery can all raise your risk of developing the structural and electrical anomalies that cause atrial fibrillation. Even in a healthy heart, a fast or slow heart rate—from exercising or sleeping, for example—can trigger atrial fibrillation.
Age
The risk of atrial fibrillation increases as you age, especially after age 65. Atrial fibrillation is rare in children, but it does occur, especially in boys and in children who have obesity.
Family history and genetics
If someone in your family has had atrial fibrillation, you have a higher risk of developing atrial fibrillation, too. Scientists have found some genes with mutations that raise the risk of atrial fibrillation. Some of these genes influence fetal organ development or heart cell ion channels. Sometimes these genetic patterns are also linked to heart disease. Some genetic factors may raise the risk of atrial fibrillation in combination with such factors as age, weight, or sex.
Lifestyle habits
Some lifestyle habits can raise or lower your risk of atrial fibrillation, including the following:
- Alcohol. Drinking large amounts of alcohol, especially binge drinking, raises your risk of atrial fibrillation. Even modest amounts of alcohol can trigger atrial fibrillation in some people.
- Illegal drugs. Some street drugs, such as cocaine, can trigger atrial fibrillation or make it worse.
- Physical activity. Some competitive athletes and people—men, in particular—participating in endurance sports or exerting themselves at work may have a higher risk of atrial fibrillation. At the same time, moderate physical activity can have a protective effect. Physical fitness appears to be linked to a lower risk of atrial fibrillation.
- Smoking. Studies have found that smoking increases the risk of atrial fibrillation. The risk appears to be higher the longer you smoke and decreases if you quit. Exposure to secondhand smoke, even in the womb, can increase a child’s risk of developing atrial fibrillation.
- Stress. Stressful situations, panic disorders, and other types of emotional stress may be linked to a higher risk of atrial fibrillation.
Other medical conditions
Many other medical conditions can increase your risk of atrial fibrillation, especially heart problems. As you age, having more than one condition may increase your risk. Conditions that raise the risk of atrial fibrillation include:
- Chronic kidney disease
- Conduction disorders
- Congenital heart defects
- Diabetes
- Heart attack
- Heart failure
- Heart inflammation
- Heart tissue that is too thick or stiff
- Heart valve diseases
- High blood pressure
- Hyperthyroidism, an overactive thyroid gland
- Ischemic heart disease
- Lung diseases, including COPD
- Obesity
- Sarcoidosis
- Sleep apnea
- Venous thromboembolism
Race or ethnicity
In the United States, atrial fibrillation is more common among whites than among African Americans, Hispanic Americans, or Asian Americans. Although people of European ancestry are more likely to develop the condition, African Americans with atrial fibrillation are more likely to have complications such as stroke, heart failure, or ischemic heart disease.
Surgery
You may be at risk for atrial fibrillation in the early days and weeks after surgery of the heart, lungs, or esophagus. Surgery to correct a congenital heart defect can also raise the risk of atrial fibrillation. This can happen years after a childhood surgery or when you have surgery as an adult to correct a lifelong condition.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3831
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2018-09-27 13:44:00.0
Types of Atrial Fibrillation
Atrial fibrillation is a type of arrhythmia. There are four main types of atrial fibrillation—paroxysmal, persistent, long-term persistent, and permanent atrial fibrillation. The type of atrial fibrillation that you have depends on how often atrial fibrillation occurs and how it responds to treatment.
Paroxysmal atrial fibrillation
You may experience a brief event—a paroxysm—of atrial fibrillation. It may pass without symptoms , or you may feel it strongly. It usually stops in less than 24 hours but may last up to a week. Paroxysmal atrial fibrillation can happen repeatedly.
You may need treatment or your symptoms may go away on their own. When this kind of atrial fibrillation alternates with a heartbeat that is slower than normal, it is called tachybrady syndrome.
Persistent atrial fibrillation
Persistent atrial fibrillation is a condition in which the abnormal heart rhythm lasts for more than a week. It may ultimately stop on its own but probably will need treatment.
Long-term persistent atrial fibrillation
With this condition, the abnormal heart rhythms last for more than a year without going away.
Permanent atrial fibrillation
Sometimes atrial fibrillation does not get better, even when you have tried several times to restore a normal heart rhythm with medicines or other treatments. At this point, your atrial fibrillation is considered permanent.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3827
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2018-09-27 13:43:00.0
Atrial Fibrillation – Signs, Symptoms, and Complications
You may or may not notice atrial fibrillation. It often occurs with no signs or symptoms. If you do have symptoms, you may notice something that occurs only occasionally. Or, your symptoms may be frequent or serious. If you have heart disease that is worsening, you may notice more symptoms of atrial fibrillation. If your atrial fibrillation is undetected or left untreated, serious and even life-threatening complications can arise. They include stroke and heart failure.
Signs and symptoms
The most common symptom of atrial fibrillation is Fatigue . Other signs and symptoms include:
- Heart palpitations
- Difficulty breathing, especially when lying down
- Chest pain
- Low blood pressure
- Dizziness or fainting
Keep track of when and how often your symptoms occur, what you feel, and whether these things change over time. They are all important clues for your doctor.
Complications
When it is undetected or untreated, atrial fibrillation can lead to serious complications. This is especially significant for African Americans. Even though whites have atrial fibrillation at higher rates, research has found that many of its complications—including stroke, heart disease, and heart failure—are more common among African Americans. Some complications of atrial fibrillation include:
- Blood clot. With atrial fibrillation, the heart may not be able to pump the blood out properly, causing it to pool and form an abnormal blood clot in the heart. A piece of the clot—a type of embolus—can break off and travel through the blood to different parts of the body, blocking blood flow to the brain, lungs, intestine, spleen, or kidneys. Atrial fibrillation may also increase the risk of venous thromboembolism, which is a blood clot that forms in a vein.
- Cognitive impairment and dementia. Some studies suggest that impaired cognition, Alzheimer’s disease, and vascular dementia occur more often among people with atrial fibrillation. This may be due to blockages in the blood vessels of the brain or reduced blood flow to the brain.
- Heart attack. The risk of a heart attack from atrial fibrillation is highest among women and African Americans and especially in the first year after atrial fibrillation is diagnosed.
- Heart failure. Atrial fibrillation raises your risk of heart failure because the heart is beating fast and unevenly. The heart’s chambers do not fill completely with blood and cannot pump enough blood to the lungs and body. Atrial fibrillation may also make your heart failure symptoms worse.
- Stroke. If an embolus travels to the brain, it can cause a stroke. For some people, atrial fibrillation has no symptoms, and a stroke is the first sign of the condition. If you have atrial fibrillation, the risk of a stroke is higher if you are a woman.
- Sudden cardiac arrest. With atrial fibrillation, there is an increased risk that the heart may suddenly and unexpectedly stop beating if you have another serious heart condition.
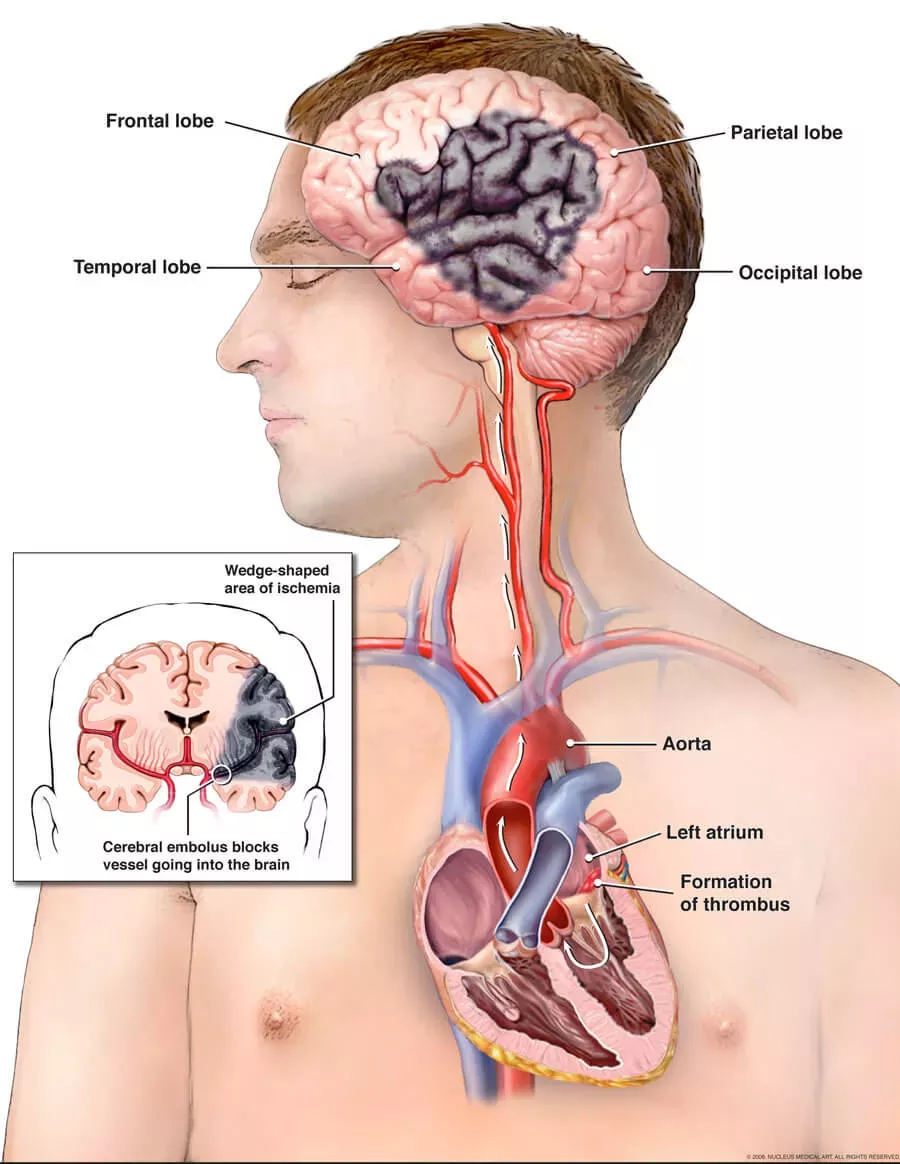
Atrial fibrillation and stroke. The illustration shows how a stroke can occur during atrial fibrillation. A blood clot can form in the left atrium of the heart. If an embolus, or a piece of the clot, breaks off and travels to an artery in the brain, it can block blood flow through the artery. The lack of blood flow to the portion of the brain fed by the artery causes a stroke. Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved.
Look for
- Diagnosis will explain tests and procedures used to detect signs of atrial fibrillation and help rule our other conditions that may mimic atrial fibrillation.
- Treatment will discuss treatment-related complications or side effects.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3832
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2018-09-27 13:46:00.0
Atrial Fibrillation Screening and Prevention
Typically doctors screen for atrial fibrillation only when you have risk factors. However, your doctor may check for signs of atrial fibrillation as part of your regular medical care. Screening tests include checking your pulse or recording your heart’s electrical activity. Your doctor may recommend healthy lifestyle changes to help you lower your risk of developing atrial fibrillation.
Screening tests and results
Screening may be part of your regular care if you are 65 or older or if you have other risk factors.
- Your doctor may check your pulse. Even without symptoms, your heart may have an irregular speed or faulty rhythm that your doctor can detect.
- If you have had a stroke and there is no clear cause, your doctor may recommend screening for atrial fibrillation with a Holter or event monitor or a loop recorder, which is a small monitor placed just under the skin of your chest.
- Several devices are now available to detect and record your heart’s rhythm similar to an electrocardiogram (EKG). These devices may also email the data to your doctor.
Prevention strategies
To help you lower your risk of atrial fibrillation, your doctor may recommend certain heart-healthy lifestyle changes, including aiming for a healthy weight, being physically active, controlling your blood sugar, limiting alcohol, lowering your blood pressure, managing stress, and quitting smoking.
In addition, some illegal drugs, such as cocaine, can trigger atrial fibrillation or make it worse. Ask your doctor for help avoiding these triggers to prevent arrhythmia.
If you are having heart surgery, your medical team will monitor you. To prevent arrhythmia, your doctor may recommend antiarrhythmic medicine or treatment to maintain or supplement electrolyte levels during or after the procedure.
Look for
- Diagnosis will explain tests and procedures that your doctor may use to diagnose types of atrial fibrillation.
- Living With will discuss what your doctor may recommend to prevent your atrial fibrillation from recurring, getting worse, or causing complications.
- Research for Your Health will discuss how we are using current research and advancing research to prevent atrial fibrillation.
- Participate in NHLBI Clinical Trials will explain our open and enrolling clinical studies that are investigating prevention strategies for atrial fibrillation.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3837
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2018-09-27 13:45:00.0
Atrial Fibrillation – Causes
Changes to the heart’s tissue and to its electrical signals most often cause atrial fibrillation. To understand atrial fibrillation, it helps to know how the heart works. When the heart’s tissue or signaling is damaged, the regular pumping of the heart muscle becomes fast and irregular. Most often, damage to the heart is the result of other conditions such as high blood pressure and ischemic heart disease. Other factors can also raise your risk of atrial fibrillation.
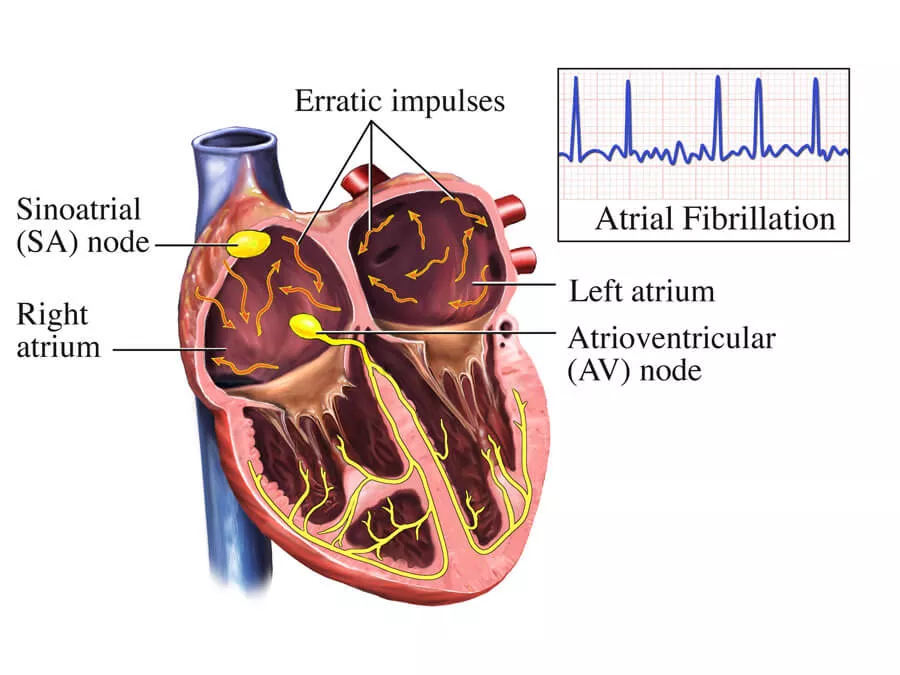
Atrial fibrillation. This image shows the electrical system of the heart during atrial fibrillation. Normally, an electrical signal at the sinoatrial (SA) node in the upper right chamber of the heart causes the upper chambers to contract and pump blood into the lower chambers. The electrical signal travels down the heart and causes the lower chambers to contract. In atrial fibrillation, abnormal electrical signals in the upper chambers overwhelm the normal signal from the SA node and cause the upper chambers to beat irregularly. This image includes a graphical representation of the EKG (ECG) showing the electrical impulses illustrated within the heart. Medical Illustration Copyright © 2019 Nucleus Medical Media, All rights reserved.
Changes in heart tissue
Usually the cells of the heart fire and contract together. However, when aging, heart disease, infection, genetic , or other factors change heart tissue, that pattern breaks down. This can happen because of fibrosis , inflammation , a thinning or thickening of the heart walls, lack of blood flow to the heart, or an abnormal buildup of proteins, cells, or minerals in heart tissue.
Changes in electrical signaling
Usually, a trigger heartbeat sets off atrial fibrillation. Electrical signals from this trigger may then cause the heart to beat slower or faster than usual because of changes in heart tissue. Sometimes, the signals create an atypical loop, telling the heart to contract over and over. This can create the fast, chaotic beating that defines atrial fibrillation.
Variations in the heart’s electrical signaling can be due to differences in heart anatomy, premature or extra heartbeats, normal heart rate adjustments, patches of faster or slower tissue, and repeated stimulation of certain tissue patches.
Look for
- Treatment will discuss medicines and procedures that your doctors may recommend if you are diagnosed with atrial fibrillation.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/3830
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2018-09-27 13:44:00.0