Science at the Heart of Medicine
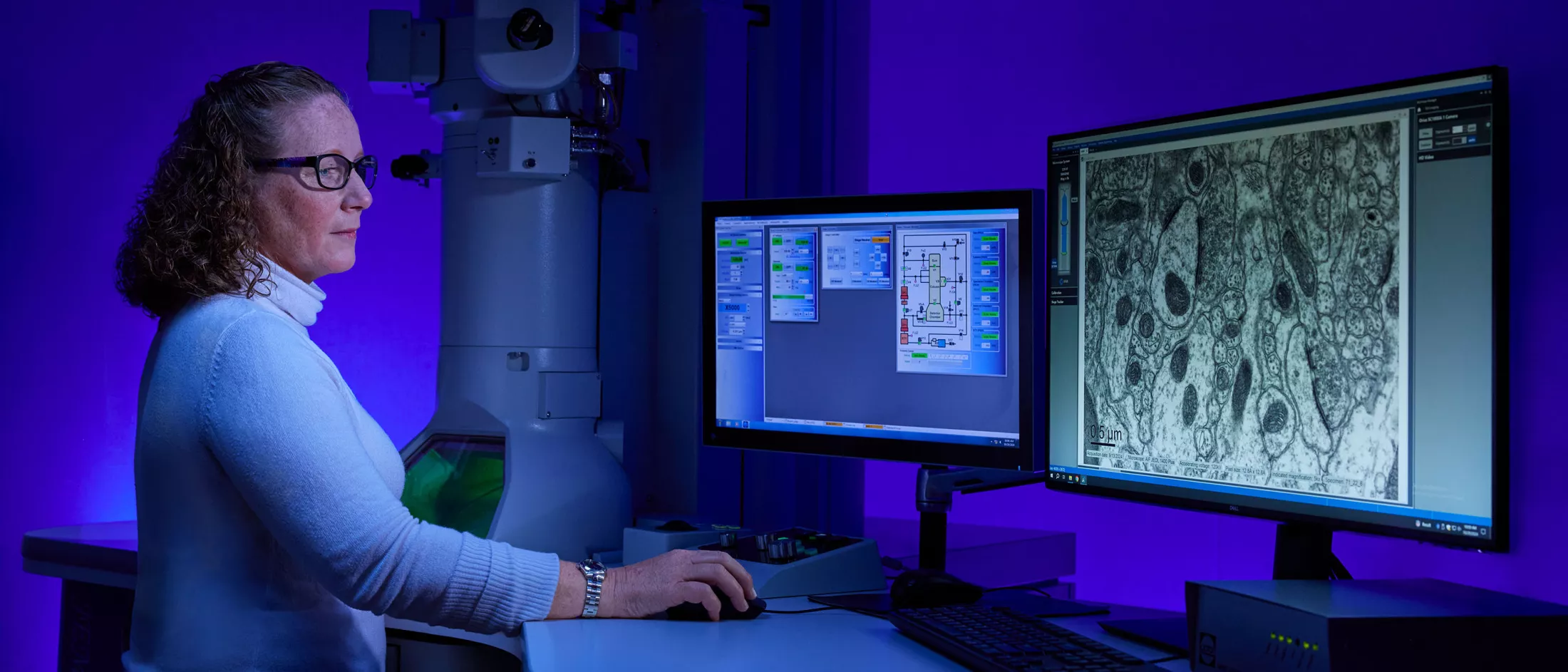
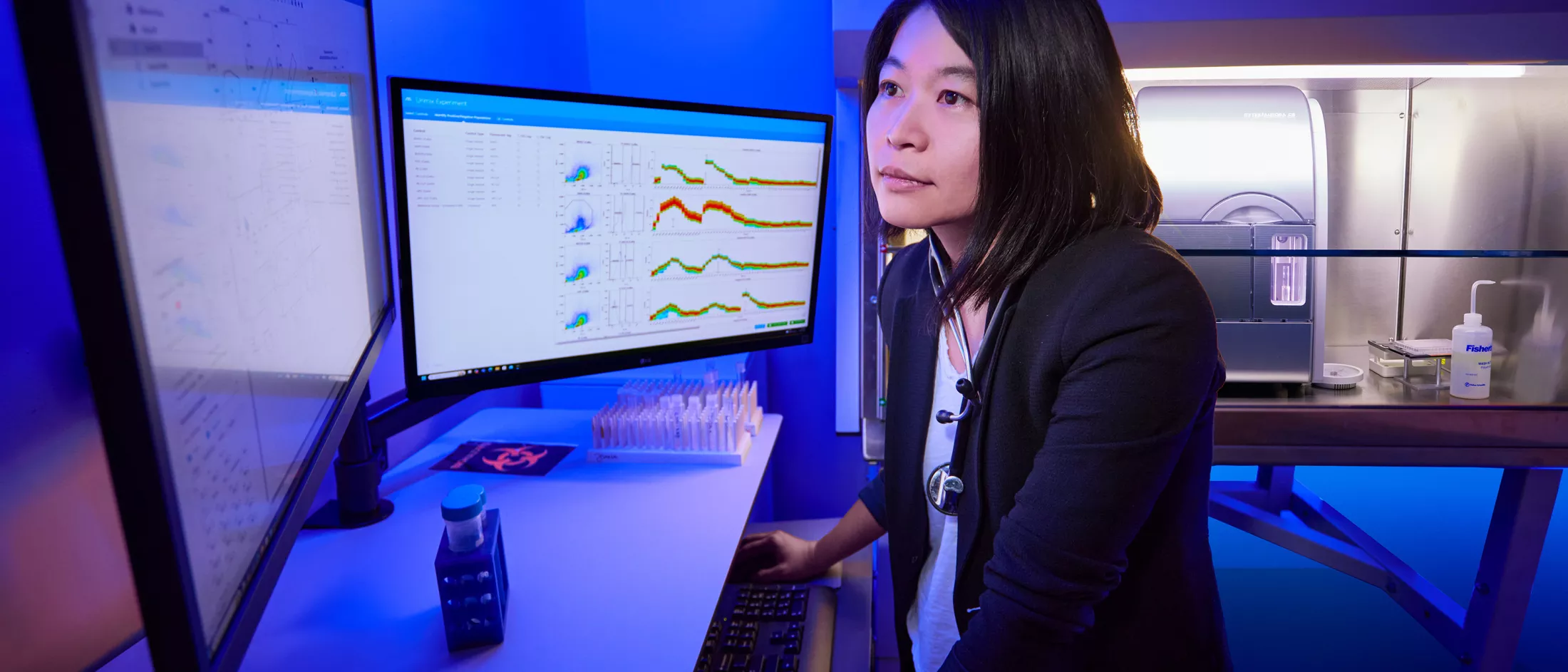
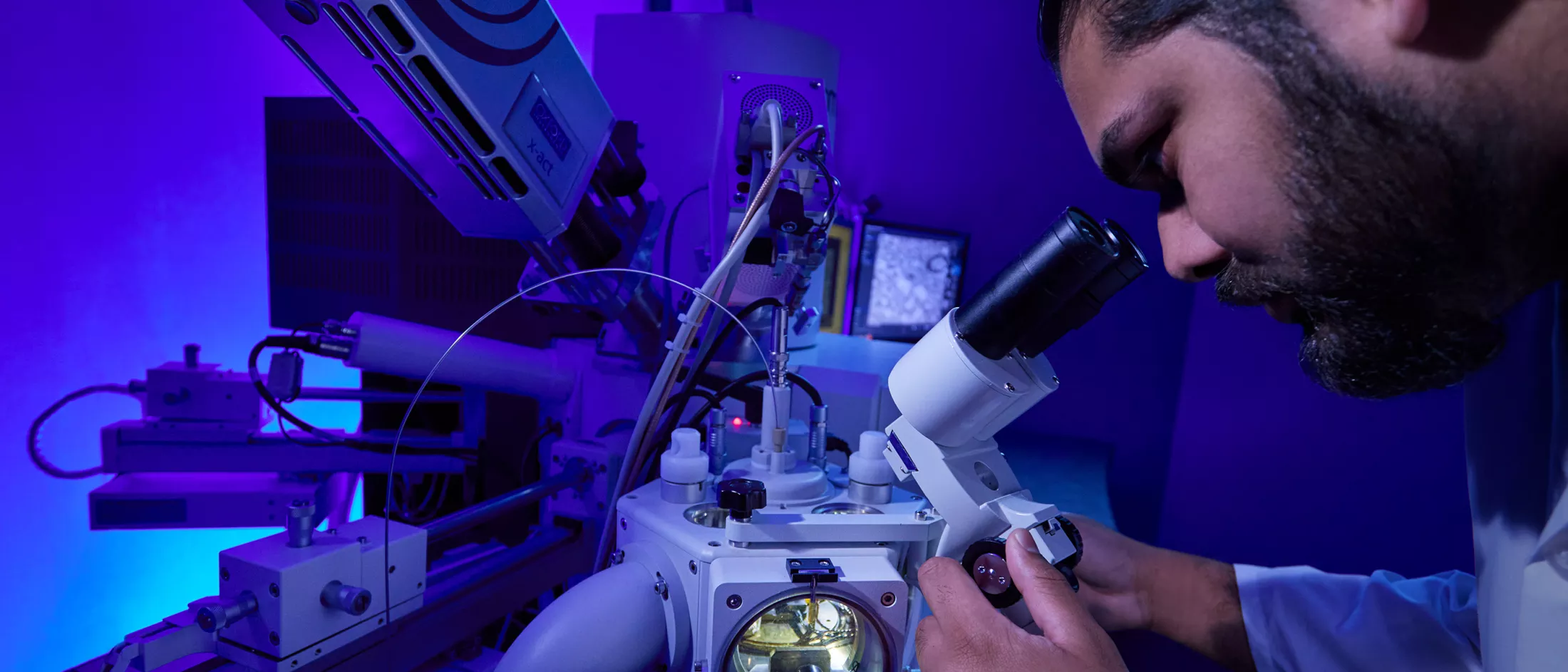
The New York Center for Rare Diseases at Montefiore Einstein is at the forefront of innovation and rare disease research, committed to finding new ways to predict, prevent, diagnose and treat rare conditions. As a National Organization for Rare Disorders (NORD)-designated Rare Disease Center of Excellence, we offer a research-focused, evidence-based approach to care. Our world-renowned physician-scientists and scientists collaborate closely across disciplines and with investigators worldwide, leading research and spearheading numerous studies and clinical trials. This gives our patients access to emerging technologies and innovative treatments and cures that may otherwise be unavailable.
Our research teams are actively conducting basic, translational and clinical research to explore the genetic mechanisms, natural history, epigenomics and population genetics of rare diseases and develop diagnostic and therapeutic solutions for a broad range of rare conditions. From co-developing the clinical guidelines setting the standard of care for acid sphingomyelinase deficiency to spearheading the nation’s largest pilot newborn rare diseases screening study (ScreenPlus), we continue to lead the way in rare disease research. We have also partnered with GeneDx, PacBio and the Genomics team in Google Research to help identify the genetic causes and best treatments for rare diseases.
Our basic science and translational research programs are focused on numerous compelling areas of rare disease research at the cellular and molecular levels. From investigating the mechanisms of human disease, transcriptional regulation and DNA sequence variation in the non-coding majority of the genome, and why rare diseases occur in an individual or family, to exploring the mechanisms responsible for birth defects in 22q11.2 deletion syndrome (22q11.2DS) and neurodegeneration in RNA polymerase III-related leukodystrophy, and developing gene therapy for hereditary red blood cell disorders, our researchers are pushing the boundaries of modern science.
Clinical Trials
We are spearheading all phases and types of clinical trials, some of which are sponsored by the National Institutes of Health (NIH), for individuals with rare diseases. By enrolling in a clinical trial, you can help our scientists develop new treatments, diagnostic tools and other strategies to prevent, diagnose and treat rare diseases. Through our clinical trials, you may also be able to access emerging technologies and innovative treatments that may otherwise not be available to the general public.

Featured Rare Disease Clinical Trials
Rett Syndrome Registry (RSR)
-
Start Date
August 2, 2022
-
Conditions
Rett Syndrome, Rett Syndrome (Atypical) , Genetic Disease, Genetic Diseases (X-Linked), Intellectual Disability, Neurobehavioral Manifestations, Neurologic Manifestations, Neurologic Disorder, Neurodevelopmental Disorders, Nervous System Diseases
ScreenPlus: A Comprehensive, Flexible, Multi-disorder Newborn Screening Program (ScreenPlus)
-
Start Date
May 10, 2021
-
Conditions
Acid Sphingomyelinase Deficiency, Ceroid Lipofuscinosis (Neuronal 2), Cerebrotendinous Xanthomatosis, Fabry Disease, GM1 Gangliosidosis, Gaucher Disease, Lysosomal Acid Lipase Deficiency, Metachromatic Leukodystrophy, Mucopolysaccharidosis II, Mucopolysaccharidosis III-B, Mucopolysaccharidosis IV A, Mucopolysaccharidosis VI, Mucopolysaccharidosis VII, Niemann-Pick Disease (Type C)
Lysosomal Acid Lipase (LAL) Deficiency Registry (ALX-LALD-501)
-
Start Date
May 30, 2013
-
Conditions
Lysosomal Acid Lipase Deficiency, Cholesterol Ester Storage Disease, Wolman Disease, Acid Cholesteryl Ester Hydrolase Deficiency (Type 2), LIPA Deficiency, LAL-Deficiency
Bronx Transthyretin Amyloid Cardiomyopathy Database
-
Start Date
September 23, 2023
-
Conditions
Transthyretin Cardiac Amyloidosis, Transthyretin Amyloid Cardiomyopathy
A Study Evaluating Gene Therapy with BB305 Lentiviral Vector in Sickle Cell Disease
-
Start Date
February 14, 2020
-
Conditions
Sickle Cell Disease
ATHN Transcends: A Natural History Study of Non-Neoplastic Hematologic Disorders
-
Start Date
September 30, 2020
-
Conditions
Hematologic Disorder, Bleeding Disorder, Connective Tissue Disorder, Hemophilia, Thrombosis, Von Willebrand Diseases, Thrombophilia, Rare Bleeding Disorder, Platelet Disorder, Factor IX Deficiency, Factor VIII Deficiency, Thalassemia, Sickle Cell Disease
MEK Inhibitor Mirdametinib (PD-0325901) in Patients with Neurofibromatosis Type 1 Associated Plexiform Neurofibromas (ReNeu)
-
Start Date
September 29, 2019
-
Conditions
Plexiform Neurofibroma, Neurofibromatosis Type 1 (NF1)
Nephrotic Syndrome Study Network (NEPTUNE)
-
Start Date
April 1, 2010
-
Conditions
Minimal Change Disease (MCD), Membranous Nephropathy, Glomerulosclerosis (Focal Segmental)