Otorhinolaryngology – Head & Neck Surgery (ORL-HNS) Education & Training
At Montefiore Einstein Otorhinolaryngology – Head and Neck Surgery (ORL-HNS), we are guided by a mission to heal, teach, discover and advance the health of the communities we serve. We are widely recognized for our expertise and innovation in medical simulation, from otorhinolaryngology boot camps to in situ training designed to improve patient outcomes. Working within our Program that cultivates a framework for lifelong learning, our otorhinolaryngology residents develop the clinical and surgical skills necessary to deliver empathetic, humble and skilled patient care. Our Program teaches state-of-the-art medicine informed by evidence and emphasizes a patient-first ethic while maintaining a healthy work-life balance. We nurture leadership and foster an investigative and curious approach to medicine. In the process, we develop skilled physicians, many of whom move on to the job or fellowship of their choice.
Clinical & Research Excellence
Our mission to improve access and quality of care for our diverse community draws residents from top medical schools around the world. We develop and expand programs designed to advance teamwork, communication and decision-making. Our focus on comprehensive care provides an ideal training ground for our residents and fellows.
Diversity of Experience
As a premier academic medical center serving the Bronx, Westchester County, Manhattan and the Hudson Valley, Montefiore Einstein offers its postgraduate trainees comprehensive exposure to diverse population and a broad spectrum of pathologies. This wide range of experiences prepares our postgraduate trainees for successful careers in their chosen field, whether in research, clinical or nonclinical settings.
Residency Programs
We offer an extensive experience across four campuses, providing care for a range of conditions, from acute to chronic, in both inpatient and outpatient settings. The Program includes comprehensive training in all aspects of otorhinolaryngology, head and neck surgery, ear, nose and throat (ENT) and subspecialties. Our Education Program utilizes the core competencies of patient care, medical knowledge, practice-based learning and improvement.

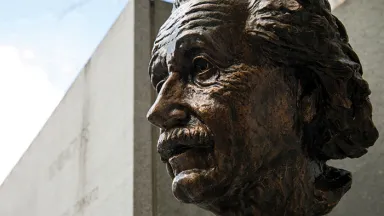
Education at Albert Einstein College of Medicine
Albert Einstein College of Medicine is a premier, research-based medical school dedicated to leading biomedical investigation and the development of ethical and compassionate physicians and scientists.