Our Approach to Movement Disorders

The Montefiore Einstein Comprehensive Movement Disorders Center is at the forefront of delivering the most advanced and innovative care for patients with all types of movement disorders. Our world-renowned, interdisciplinary specialists have among the most diverse expertise in a spectrum of related disorders, including Parkinson’s disease and related conditions, essential tremor, dystonia, tardive dystonia or dyskinesia, Tourette’s syndrome, spasticity, and other movement disorders. These conditions can result from various causes, including genetic factors, infections, trauma, metabolic abnormalities, and neurodegenerative processes.
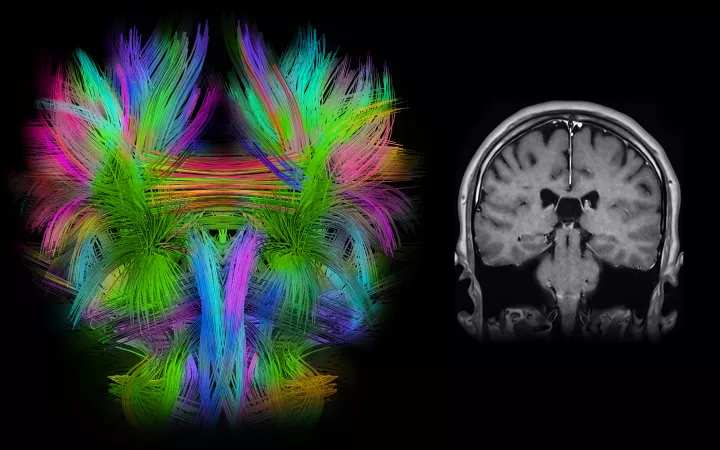
We utilize advanced technologies, including precise minimally invasive surgical placement of electrodes into brain areas uniquely involved in mediating specific movement disorders, along with subsequent programming and refinement of stimulation parameters to optimally treat individual conditions. We are ranked in the top 1% of all hospitals in the nation for neurology and neurosurgery, according to U.S. News & World Report, and an international referral site for complex and challenging movement disorder cases.
Our highly specialized team of leading experts from neurology, neurological surgery, neuroradiology, cognitive neuroscience, neurorehabilitation and biotechnology works together through consensus conferences and precision medicine initiatives, integrating AI into a comprehensive management plan to optimize functional recovery and avoid debilitating side effects often associated with medical management alone.

Leading-Edge Surgical Management
The most common movement disorders are Parkinson's disease, essential tremor, and dystonia. Medical therapy is the first line of treatment for all three conditions, but there are also effective surgical treatments in circumstances where medical therapy fails to control the symptoms or is associated with unacceptable side effects.
Parkinson’s disease (PD) is a relatively common movement disorder that gets progressively worse over time. Humans have a limited number of neurons that generate the neurotransmitter dopamine. With age, some of these neurons are progressively lost. In some individuals, dopaminergic neurons are lost at a higher-than-normal rate, leading to PD. Affected individuals may notice problems with slowing of movement (bradykinesia), tremor, stiffness or rigidity in the limbs or the trunk of the body, and/or impaired balance. As symptoms progress, people may have difficulty walking, talking or completing other simple tasks. Not everyone with one or more of these symptoms has PD, as the symptoms appear in other diseases, as well.
Effective medical treatment of PD usually entails medications that increase the amount of dopamine in the brain. These medications can be very effective, at least initially. However, after several years, the medications may become less effective or difficult to manage. Patients may develop on-off fluctuations (wherein they only have good symptom control for a brief period after taking the medications, then rapid development of symptoms as the medications wear off) or dyskinesias (excessive movements after taking the medications). These patients are then candidates for movement disorders surgery–typically deep brain stimulation or (DBS).
DBS is a surgical procedure that involves implanting electrodes into specific areas of the brain to help regulate abnormal brain activity and alleviate symptoms associated with PD. There are two FDA-approved targets for the treatment of PD: the Globus pallidus internus (GPi) and the subthalamic nucleus (STN). The decision to recommend surgery and identification of the target is made after a careful evaluation by an experienced movement disorders team. Patients being considered for DBS have a history of PD responsive to medications for 3-5 years.
Individuals who, despite optimal medication management, experience motor fluctuations, including wearing off of medication effectiveness and on-off fluctuations, are good candidates for DBS. When there is a presence of dyskinesias (involuntary movements) that are troublesome and impact the quality of life, especially if they are not well-controlled with medication adjustments, DBS is an effective treatment. DBS should be considered by those experiencing intolerable side effects from Parkinson’s medications resulting in limited use or effectiveness, as well as those experiencing significant functional impairment in daily activities despite optimal medical management.
Before considering DBS, a thorough evaluation is conducted by a team of specialists, including a movement disorders neurologist, a neuropsychologist, and a specialized neurosurgeon The movement disorders neurologist determines the accuracy of the diagnosis and optimizes the medications. The neuropsychological evaluation determines whether there are cognitive issues beyond what is expected, which may increase the risks of surgery. The neurosurgeon assesses the overall appropriateness of surgery and whether there are any medical or surgical concerns. A high-quality MRI–used to ensure that there are no significant brain abnormalities –is another important element of surgical planning. All the data is then reviewed at a multidisciplinary clinical conference, and treatment recommendations are determined.
The choice between targeting the globus pallidus internus (GPi) or the subthalamic nucleus (STN) for deep brain Stimulation (DBS) in Parkinson’s disease depends on various factors, and both targets have been shown to be effective in alleviating motor symptoms. The decision is often based on the patient’s specific clinical features, symptoms, and individual considerations.
GPi DBS may be considered when the primary goal is to control medication-induced dyskinesias (involuntary movements), for individuals experiencing medication-related side effects, and for those where there are concerns about potential cognitive or neuropsychiatric side effects associated with DBS.
STN DBS may result in greater improvement in overall motor symptoms, including tremors, bradykinesia, and rigidity. Likewise, this procedure may result in a reduction in medication doses, potentially leading to a decrease in medication-related side effects, such as levodopa-induced dyskinesias. This makes STN DBS a suitable choice for individuals who primarily seek relief from these complications.
Deep brain stimulation is a minimally invasive procedure that involves placement of one or two thin wires or electrodes into parts of the brain, or nuclei, that are known to have abnormal patterns of activity in particular movement disorders. The procedure is normally performed in two stages. In the first stage, electrodes are implanted into the GPi or the STN. This procedure is usually performed with the patient awake but lightly sedated to obtain appropriate neural recordings and to ensure that stimulation through the electrodes alleviates the symptoms. The second stage takes place one or two days later and consists of connecting the electrode wires to a small pulse generator (very similar to a pacemaker) which is implanted below the clavicle. This is a short procedure performed with anesthesia. After the surgery, the movement disorders neurologist adjusts the stimulation parameters, such as frequency, voltage, and pulse width, to achieve the best therapeutic effect with minimal side effects.
DBS surgery typically results in significant improvement in tremors, rigidity, and bradykinesia, a reduction in medication requirements (leading to fewer medication-related side effects), and an improved quality of life for most individuals. DBS may not be suitable for everyone, and individual responses to the procedure can vary. Individuals considering DBS surgery should have a comprehensive evaluation by a specialized movement disorders team to determine if they are a suitable candidate for the procedure. The decision to undergo surgery should be based on a careful consideration of potential benefits and risks, taking into account the impact of PD on the individual’s quality of life.
In addition to Parkinson’s disease, essential tremor (ET) is another common movement condition characterized by involuntary rhythmic shaking or trembling, primarily in the hands and arms (though it can affect other parts of the body, such as the head, voice or legs). Unlike Parkinson’s disease, essential tremor is often not associated with other movement symptoms.
The type of tremor primarily associated with essential tremor disorder is typically a rhythmic, back-and-forth movement that occurs when the affected part of the body is in use. This involuntary movement tends to worsen with additional movement and can be exacerbated by stress, fatigue, or certain substances like caffeine.
Essential tremor is often a progressive condition, meaning that symptoms may worsen over time. However, the rate of progression can vary among individuals. There is often a genetic component to essential tremor; it can run in families, and individuals with a family history of tremors may be at a higher risk of developing the condition. While essential tremor is not life-threatening, it can significantly impact a person’s quality of life, particularly in tasks that require fine motor skills, such as writing, eating or buttoning a shirt.
The first line of treatment is medical therapy using beta-blockers and anticonvulsants. Over time, many patients find that these medications do not adequately control the tremor or that they have unacceptable side effects. These individuals are likely candidates for DBS surgery.
As with treatment for Parkinson’s disease, ET patients considering DBS should be thoroughly evaluated by a team of specialists, including a movement disorders neurologist, and neuropsychologist and a specialized neurosurgeon. A high-quality MRI–used to ensure that there are no significant brain abnormalities–is an important element of surgical planning. DBS involves implanting electrodes into a nucleus called the thalamus to help regulate abnormal brain activity and alleviate symptoms associated with ET. There is only one established and FDA-approved target for the treatment of ET, called the Ventralis intermedius nucleus (Vim), found within the larger thalamus.
For most ET patients, DBS surgery typically results in a dramatic improvement in tremors, a reduction in medication requirements, fewer medication-related side effects, and an improved quality of life.
Dystonia is a neurological movement disorder characterized by sustained muscle contractions, resulting in repetitive, twisting, and abnormal movements or postures. These muscle contractions can be painful and may affect one specific part of the body (focal dystonia), multiple adjacent parts (segmental dystonia), or the entire body (generalized dystonia). Dystonia-associated muscle contractions can cause abnormal movements, postures, or both. These contractions can be intermittent or constant, can affect various parts of the body, including the neck (cervical dystonia or spasmodic torticollis), face (cranial dystonia), hands (writer’s cramp) and vocal cords (spasmodic dysphonia), and may worsen with stress, fatigue, or specific activities.
Dystonia can develop at any age, and its onset can be sudden or gradual. The severity and progression of symptoms can also vary widely among individuals. Some forms of dystonia are task-specific, meaning that symptoms are triggered or exacerbated by specific activities. For example, writer’s cramp involves dystonic contractions during writing. DYT1 dystonia, also known as early-onset torsion dystonia, may affect various parts of the body. DYT1 dystonia is caused by a mutation in the TOR1A gene, located on chromosome 9. which is inherited in an autosomal dominant manner, meaning that an affected person has a 50% chance of passing the condition on to each of their children.
Symptoms of DYT1 dystonia usually manifest in childhood or adolescence, typically between the ages of three and 16, but the age of onset can vary, and some individuals may not exhibit symptoms until later in life. The severity of symptoms can vary widely, even among individuals within the same family. DYT1 dystonia is generally progressive, meaning that symptoms worsen over time, and, in some individuals, may become severely disabling.
There is no cure for dystonia, though treatment options , including oral medications and botulinum toxin injections, may help manage symptoms. Patients with severe focal or generalized dystonia can obtain significant benefit from deep brain stimulation (DBS) surgery.
As with Parkinson’s disease and ET, after the surgery, the DBS system is carefully programmed by the movement disorders neurologist to achieve the best therapeutic effect with minimal side effects. Unlike PD and ET, where the effects of DBS surgery can be observed immediately, for patients with dystonia, the beneficial effects are not observed until several months after the system has been activated, at which time most individuals experience a dramatic improvement in dystonic movements and improved quality of life.
Innovative Surgical Solutions
Montefiore Einstein has developed several effective neurosurgical treatments for movement disorders. By improving our understanding of basal ganglia circuitry and evolving neurosurgical techniques, we have contributed greatly to how treatment is approached both in our center and in care facilities worldwide. With each discovery, we will move closer to fully restoring function for patients with Parkinson’s disease, dystonia, or tremors.

Your Comprehensive Movement Disorders Center Team
Our multidisciplinary team of movement disorder experts is at the forefront of movement disorder care and the development of therapies through a better understanding of the interrelationships between movement disorders and neuromuscular disorders, as well as between movement disorders and psychological conditions. Our specialists also have a keen interest in the genetics of movement disorders. From prevention to treatment options, we will propose an individualized treatment plan that fits your needs and lifestyle.
About Parkinson’s Disease
Parkinson's disease (PD) is a movement disorder of the nervous system that gets progressively worse over time. Humans have about 200,000 dopaminergic neurons at baseline. With age, some of these neurons are lost. In some individuals, dopaminergic neurons are lost at a higher-than-normal rate, leading to PD. Affected individuals may begin to notice problems with slowing of movement, tremor, stiffness or rigidity in the limbs or the trunk of the body, or impaired balance. As symptoms progress, people may have difficulty walking, talking or completing other simple tasks. Not everyone with one or more of these symptoms has PD, as the symptoms appear in other diseases as well. Hence, an important facet of optimizing care is to arrive at an accurate diagnosis, whether it is PD or another disorder.
About Dystonia
Dystonia is a neurological movement disorder characterized by involuntary or unintended muscle contractions that cause intense and sustained movements or abnormal postures that can, at times, be painful. There are several different forms of dystonia that may affect only one muscle, groups of muscles or muscles throughout the body. The affected areas and severity of symptoms vary from person to person. Some types of dystonia are heritable or genetic, while others arise without a known genetic predilection. Accurately diagnosing the type of dystonia is an important first step in providing the most effective treatment.