Our Approach to Neurovascular Conditions



The Montefiore Einstein Comprehensive Neurovascular Center is one of the leading destinations worldwide for the management of vascular diseases of the brain and spine, including ischemic and hemorrhagic strokes, venous occlusive disease, vascular malformations, subarachnoid hemorrhages, traumatic injuries and congenital conditions. We are the first health system from the Bronx to the Hudson Valley to have earned the prestigious Comprehensive Stroke Center designation from the Joint Commission and are among the top three percent of hospitals in the nation to earn this designation. We are the highest-volume stroke center in the New York metropolitan region and treat one of the most diverse communities in the nation, including pediatric and adult stroke patients, with state-of-the-art care and emerging technology. We are ranked in the top 1% of all hospitals in the nation for neurology and neurosurgery, according to U.S. News & World Report.
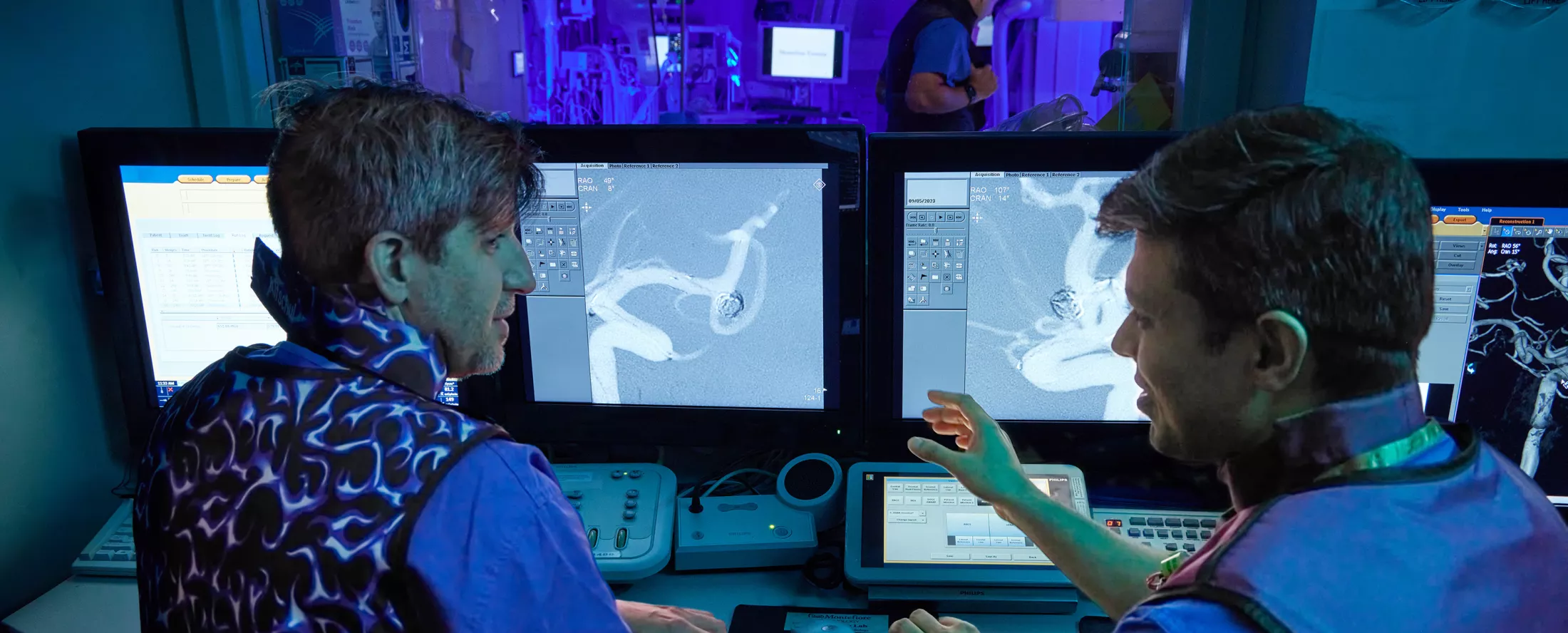
We use the latest and most advanced imaging tools and procedures to treat patients of all ages suffering from complex, life-threatening neurovascular conditions. Our neurovascular program offers a complete array of state-of-the-art solutions for the full spectrum of neurovascular diseases, including endovascular, open, minimally invasive, and hybrid surgeries.
Leading Stroke Research, Clinical Trials & Education
An internationally recognized leader in stroke research, Montefiore Einstein is a founding partner and key member of the New York City Collaborative Regional Coordinating Center (NYC-RCC), the largest National Institutes of Health (NIH)-funded, multi-institutional consortium dedicated to stroke prevention, treatment, education and rehabilitation efforts to reduce the burden of stroke on children and adults throughout the country. Distinguished as an NIH StrokeNet Regional Coordinating Center since the inception of the NIH StrokeNet in 2013, we are among an elite group of only 27 centers in the nation to be awarded a five-year grant, funded by the National Institute of Neurological Disorders and Stroke (NINDS)/NIH. We spearhead and participate in numerous clinical trials to advance promising interventions for stroke prevention, treatment, recovery and rehabilitation for patients with or at risk of a stroke across all stages of life.
A collaborative effort between the NIH and Montefiore Einstein, the Icahn School of Medicine at Mount Sinai, New York University School of Medicine and other affiliated institutions and partner sites, our Regional Coordinating Center encompasses all boroughs of New York City, Westchester, Long Island and Upstate New York, as well as Nashville, TN, and we continue to expand our network. We also continue to develop interdisciplinary endovascular platforms, new devices and intersectional strategies for conducting ultra-rapid clinical trials.
At the Montefiore Einstein Comprehensive Neurovascular Center we are also leaders in education, advancing programs and training for the next generation of top multidisciplinary experts in stroke care.
Recognized Expertise
The Montefiore Einstein Comprehensive Neurovascular Center team is led by nationally renowned vascular neurologists, neurosurgeons and neuroradiologists. Our multidisciplinary team members have advanced fellowship training, experience and expertise in the latest technologies and techniques for treating strokes, aneurysms and vascular malformations, among other conditions. We are also one of few centers in the nation whose specialists in all three departments have been trained through fellowship programs focused on endovascular techniques.
Advanced Treatments
The Montefiore Einstein Comprehensive Neurovascular Center team is led by nationally renowned vascular neurologists, neurosurgeons and neuroradiologists. Our multidisciplinary team members have advanced fellowship training, experience and expertise in the latest technologies and techniques for treating strokes, aneurysms and vascular malformations, among other conditions. We are also one of few centers in the nation whose specialists in all three departments have been trained through fellowship programs focused on endovascular techniques.
Patients are initially evaluated by neurologists with subspecialty training in stroke and endovascular neurology. They will determine if the patient needs urgent medical treatment, minimally invasive endovascular treatment, or open surgical or neurosurgical treatment.
Aneurysms
There are a range of surgical options for treating aneurysms, each with its own benefits and requirements for postoperative follow-up and care. Based on an individualized approach, each patient’s unique needs are considered during the consultation to determine the most promising outcome.
Surgical clipping is a tried and tested treatment for brain aneurysms. Benefits for patients who undergo surgical clipping include a durable, immediate cure with little risk for recurrence and little long-term follow-up care required. This procedure involves a skin incision behind the hairline and a craniotomy in which a window of bone is removed from the skull using a special, medical drill. A surgical microscope is used to maneuver in between the bone and brain to pinch off the aneurysm with a surgical clip. Surgical clipping is an excellent treatment option for aneurysms which are easy to access surgically, as well as aneurysms with a wide opening. On rare occasions, bypass surgery is required in addition to clipping.
Another minimally invasive and safe surgical option is endovascular coiling. A long plastic tube, called a microcatheter, is used to travel from an artery in the leg or wrist into the affected artery in the brain and to block off the aneurysm by filling it with platinum wires called coils. Coiling is a very safe and effective treatment for brain aneurysms, particularly for aneurysms with narrow openings or necks and wide waists or domes. This approach is often safer for aneurysms located in the vertebrobasilar system or posterior circulation. Endovascular coiling has a rapid recovery time, but there is a 15% chance of aneurysm recurrence following this procedure, so regular, follow-up monitoring is needed.
For aneurysms with wider openings or necks, there are two approaches that are more complex but still minimally invasive and involve additional support for the coils (in cases where aneurysms cannot be coiled alone). Both balloon assisted coiling and stent assisted coiling have proven benefits and rapid recovery times. A stent is a permanent scaffold to support coils, while a balloon is a temporary one. A stent calls for two additional medications that block platelet function to be taken for three to six months following the procedure. These medications are not required following the balloon procedure.
In cases of fusiform and wide-necked, side-wall aneurysms that cannot be coiled, flow diverter stenting is an extremely effective and minimally invasive treatment. This procedure uses a finely-woven stent which treats brain aneurysms without manipulating the aneurysm at all. The stent works best for aneurysms off of the internal carotid artery and requires patients to take two additional medications to block platelet function for six months.
There are currently four different flow-diverter stents that are FDA-approved in the United States. They differ slightly in size, length, outward force and stiffness. The choice of stent requires expertise and experience using both. These stents have higher cure rates than coiling approaches, with cure rates of 90% at one year, and 95% at three years following the procedure.
There is currently one endovascular flow disruptor device available in the United States, called the WEB device. It was approved in 2019 and is a minimally invasive approach used to treat aneurysms with shapes that cannot be coiled. The WEB is a finely-woven, basket-shaped device that is designed to treat wide opening or necked bifurcation brain aneurysms. The WEB acts like a flow diverter, but it is placed inside the aneurysm. This innovative device is designed to treat aneurysms past the internal carotid artery and does not require dual antiplatelet blood thinner medication.
Arteriovenous Malformations
For patients with arteriovenous malformation (AVM), the following treatment options can achieve a stand-alone cure. However, a combined approach is often most effective. The goal of any treatment option is to completely disconnect the connections to achieve a total cure. Only a total cure will eliminate the risk of bleeding.
The surgical treatment option with the highest cure rates is open surgical resection of brain arteriovenous malformations, with success dependent upon the location of the AVM and its proximity to eloquent brain areas (areas of the brain that control important neurologic functions, such as visual perception, language, and movement centers). While this procedure is more invasive, it has immediate results and provides a lasting cure.
Important factors in determining whether this procedure is the best treatment option include age, the size of the nidus, and whether there is a vein that drains into the deep venous system. Surgery involves a skin incision, a craniotomy (removing a window of bone from the skull using a medical drill), and a surgical microscope that is used to carefully disconnect and remove the AVM nidus.
Another surgical option for AVMs is embolization. This method involves inserting a long plastic tube, called a microcatheter, into either the feeding artery or draining vein and injecting a liquid embolic agent or medical-grade “crazy glue” to disconnect the abnormal connections. While embolization is minimally invasive and can make surgery easier by taking away some of the blood supply, it has the lowest cure rates and is not commonly used as a stand-alone treatment.
In certain situations, embolization can be curative when there is a singular arterial blood supply, and it may be optimal for deep, small AVMs that have bled. The transvenous approach (going through the vein to block the AVM) has not been studied well in comparison to other standard treatments, but it is a promising new technique with potentially high cure rates.
For small, deep-located AVMs, stereotactic radiation surgery (SRS) is a noninvasive procedure that involves delivering focused, high-intensity radiation to the AVM nidus. This treatment is performed in cooperation with a radiation oncologist. The neurosurgeon uses special diagnostic imaging studies to define a target in three-dimensional space. The radiation oncologist and radiation physicist then create a radiation plan to deliver the radiation dose to the specified area. This treatment is specifically highly effective for AVMs with a nidus smaller than 3cm. It typically takes three to five years to achieve a cure.
Sometimes, an AVM requires a combination of therapies to achieve the best possible chance at a cure. The most common combination of procedures is embolization followed by surgery. However, there are times when embolization can be combined with SRS or SRS can be combined with surgery. Often these combinations might be necessary for larger size AVMs. The order in which these treatment combinations are offered requires expert clinical judgment. Embolization and SRS can also be offered in a staged approach, requiring multiple treatments. Again this is more commonly required in larger size AVMs.
Moyamoya Disease
Some rare conditions cannot be fully cured, as they interfere with blood vessels (internal carotid arteries) that supply blood to the brain. One such diagnosis is Moyamoya disease, which results in an increased risk of stroke and brain bleeding. However, patients diagnosed with Moyamoya disease may benefit from surgery that can reduce these risks.
There are different surgical options for Moyamoya patients, including superficial temporal artery to middle cerebral artery (STA-MCA) bypass surgery, encephaloduroarteriosynangiosis (EDAS), encephaloduroarteriomyosynangiosis (EDAM) and multiple burr hole surgery. EDAM and multiple burr hole surgery tend to be reserved for situations when there is no obvious donor artery available, or for patients that continue to have symptoms after revascularization surgery.
STA-MCA bypass involves dissecting the artery of the scalp, making a craniotomy (removing a window of bone from the skull using a medical drill), and surgically connecting this artery to the artery of the brain. This procedure has promising long-term results, and immediately restores blood supply to the brain.
An encephaloduroarteriosynangiosis EDAS procedure involves dissecting the artery of the scalp, making a craniotomy (removing a window of bone from the skull using a medical drill), and laying the scalp artery onto the surface of the brain and letting the artery grow a new connection to supply blood to the brain over time. This method does not require temporary occlusion of the brain artery.
Research & Clinical Trials
An NIH StrokeNet Regional Coordinating Center, Montefiore Einstein Comprehensive Stroke Center participates in several NIH- and industry-funded stroke clinical trials and registries. In 2020, the vascular neurology and neurological surgery faculty published 30 articles in peer-reviewed journals, including many describing the novel aspects of stroke associated with COVID-19.

Your Comprehensive Neurovascular Center Team
About Stroke & Other Neurovascular Conditions
Neurovascular disorders, including brain aneurysms, arteriovenous malformations (AVMs), carotid artery disease, and intracranial atherosclerotic disease are conditions that affect the blood supply to the brain or spinal cord. Blockages in the arteries leading to the brain can then lead to a range of neurological problems–from a stroke to disability and even death. Neurovascular disease is a leading cause of disability in adults.
A stroke is a brain attack. It is a sudden interruption of continuous blood flow to the brain and a medical emergency. A stroke occurs when a blood vessel in the brain becomes blocked or narrowed, or when a blood vessel bursts and spills blood into the brain. Just like a heart attack, a stroke requires immediate medical attention.