Leading-Edge Research Dedicated to Epilepsy Patients
The Epilepsy Division is dedicated to advanced clinical and preclinical translational research that furthers care and treatment for people with seizures and epilepsy across the lifespan, as well as training future epileptologists to provide excellent clinical care and state-of-the-art research. There is an extensive international network of collaborative clinical and preclinical multicenter research studies, many of which are led by Montefiore Einstein investigators.
Areas of Concentration
Our investigative spectrum includes research that aims to better understand the role that genetics play in epilepsy; examines the pathophysiology of seizures—as well as of the etiologies and consequences of seizures—and evaluates new treatments for patients with seizures. Our specific areas of interest include the following:
- Drug-resistant epilepsies
- Post-traumatic seizures and epilepsy
- Infantile and epileptic spasms syndrome
- Neonatal seizures
- SARS-CoV-2
- Epilepsy genetics
- Seizure precipitants and forecasting
- Stress and epilepsy
Current Research Projects & Highlights
Our current projects include the following:
- Clinical trials for new treatments for drug-resistant epilepsies. Our current trials include:
- "Investigate Efficacy and Safety of Carisbamate as Adjunctive Treatment for Seizures Associated with LGS in Children and Adults": This is a multicenter study evaluating the efficacy of a novel antiseizure medication for the treatment of drop seizures in children and adults with Lennox Gastaut Syndrome.
- "A Randomized Study of XEN1101 Versus Placebo in Focal-Onset Seizures": This is a multicenter study investigating the efficacy, safety and tolerability of a novel potassium channel opener for the treatment of focal onset seizures.
- Identification of new therapies and biomarkers for infantile and epileptic spasms syndrome targeting spasms, associated epilepsies as well as neurodevelopmental consequences, using multicenter research collaborations. These are some examples:
- Our center has provided proof-of-concept preclinical evidence for two medications that have been subsequently designated orphan drugs for infantile and epileptic spasms.
- Preclinical trials identified treatments with potential to stop epilepsy development in a model of infantile and epileptic spasms.
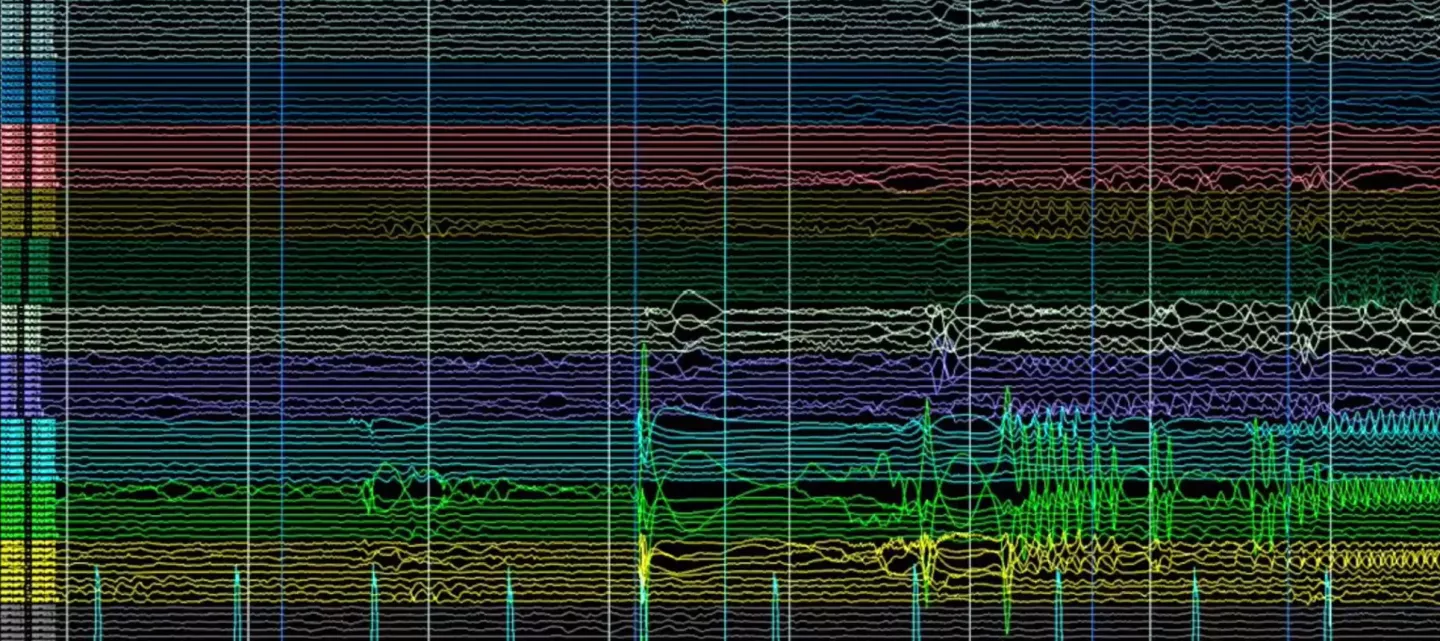
- We have developed electroencephalography (EEG)-based methods for early detection of spasms and exploration of brain networks involved in the generation of spasms.
- Ongoing preclinical trials explore the value of novel investigative drugs in the treatment of infantile and epileptic spasms.
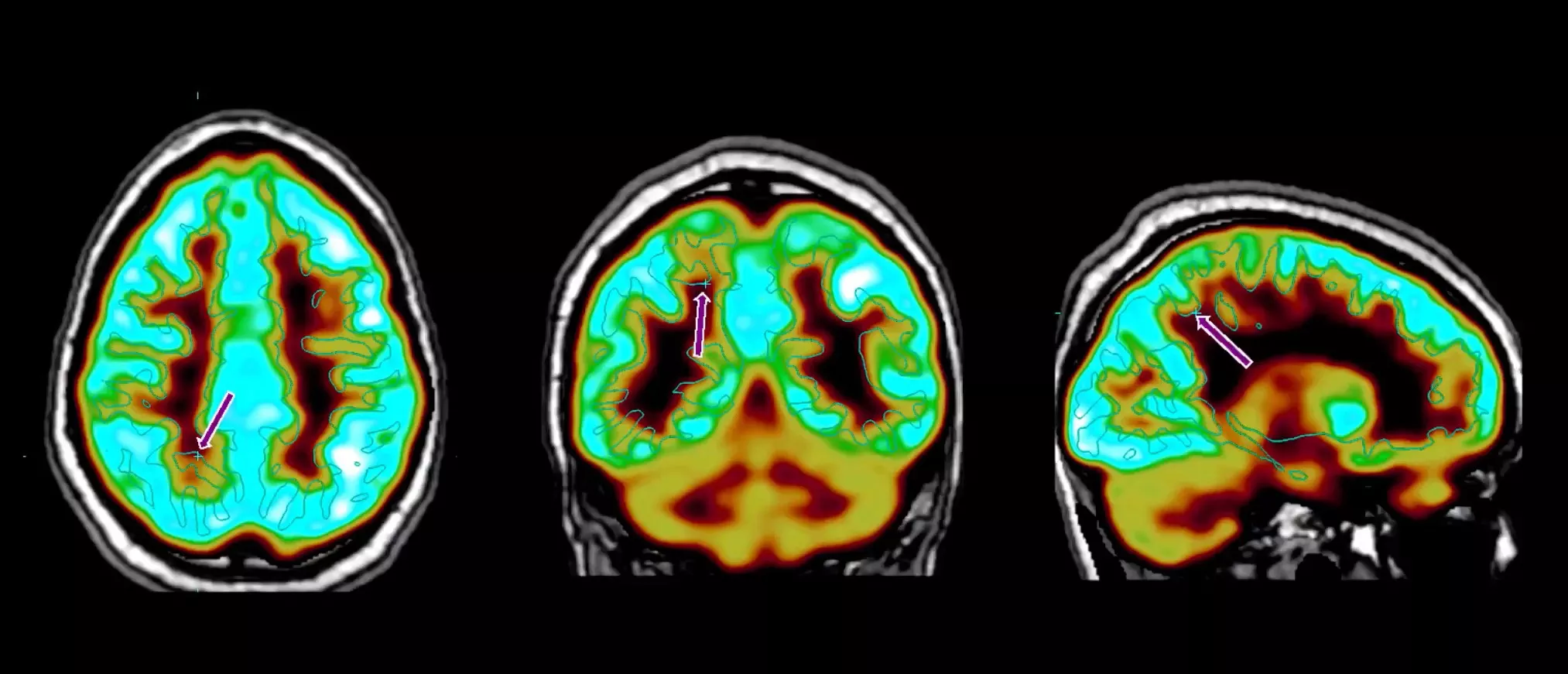
- Identification of individualized, biomarker-guided treatments for the prevention of post-traumatic epilepsy. Such studies have been funded by the NINDS and US Department of Defense.
- Our center leads international multicenter research collaborations for the development and validation of multimodal biomarkers predicting early and late seizures, neuromotor recovery and treatment response after brain trauma, as well as screening for therapies that prevent post-traumatic epilepsy. An example of this collaboration would be the Epilepsy Bioinformatics Study for antiepileptogenic therapy (EpiBioS4Rx), the first center without walls funded by NINDS.
- We provided evidence that incorporation of clinical parameters is critical for the correct interpretation of biomarkers. Based on this we have created:
- A multicenter, international research collaborative utilizing a translational platform for multimodal biomarker and treatment discovery for post-traumatic epilepsy (NINDS RO1 funded).
- Optimized models for the study of post-traumatic epilepsies and sequelae, and their biomarkers and treatments (US Department of Defense funded multicenter studies).
- Studies on the neurological sequelae of SARS-CoV-2 infection in critically ill patients:
- We provided the first evidence on high rates of EEG epileptiform abnormalities in critically ill patients with SARS-CoV-2.
- Ongoing studies assess the neurological sequelae of hospitalized patients with SARS-CoV-2 infection.
- Pioneering studies on seizure precipitants and self-seizure forecasting with a focus on stress:
- We co-directed the largest randomized trial of stress reduction for the treatment of refractory epilepsy.
- We are in the forefront of using smartphone technology towards experience-based sampling of mood and other precipitants of epilepsy.
- We are currently expanding the study of stress and seizure forecasting to include biomarkers and daily physiologic measures of stress.
- Our faculty members have played leading roles in international initiatives to provide best practices and infrastructure, transforming the clinical management and research practices which ultimately translate into better diagnoses and therapies for patients with seizures across their lifespan. Examples include:
- Classification or seizures, epilepsies and epilepsy syndromes
- Classification of neonatal seizures
- Standardization of EEG practice and interpretation in preclinical and clinical studies
- Development of common data elements for epilepsy research studies to facilitate data sharing, collaborations, and data validation
- Pioneered studies on subcortical networks, as well as age and sex-specific factors influencing seizure susceptibility and the consequences of seizures on brain development.
- Provided proof of concept for the role of brainstem structures, like the substantia nigra pars reticulata, in seizure control.
- First evidence of the role of neurotransmitter signaling systems, like GABAA receptors, on sexual differentiation of the brain.
- NS-PEACE: Neonatal Seizures—Predicting Epilepsy and Assessing Comparative Effectiveness. NIH-funded multicenter observational research to study the:
- best second-line anti-seizure medication for acute neonatal seizures (phenytoin/fosphenytoin vs levetiracetam)
- potential for subsequent chronic use of sodium channel blockers (i.e., oxcarbazepine) to increase the risk for infantile spasms syndrome, and
- reliability and validity of our published model to predict epilepsy among neonates with acute symptomatic seizures who survive into infancy.
We are also engaged in active research initiatives focused on the social determinants and barriers in the implementation of clinical care and research; epilepsy genetics; Rett syndrome; neonatal seizures; use of electronic medical records for epilepsy research; as well as the study of the relationship between stress and epilepsy.