Our History, as Written
by Dr. Isabelle Rapin
The most salient feature of the early Neurology Department was that, within less than five years, it had attained national and international status. What made it so? Its rocket ascent can be attributed to two interlocking features. The first was that when the Albert Einstein College of Medicine (Albert Einstein College of Medicine) was conceived, anti-Semitism in academe was still alive and thriving. As a result, the infant College was able to recruit a stellar faculty attracted by its charter with a clear statement of non-discrimination. The same charter also may have influenced Albert Einstein to lend his name to this non-sectarian branch of a Jewish university. The second feature was the extraordinary coup of the Professor and Chairman of Medicine, Irving London, himself a distinguished clinician/investigator, when he recruited Saul R. Korey to chair the Division of Neurology in Medicine. This was done with the understanding that neurology would become an independent department when it had accrued sufficient faculty and a residency program. Yeshiva President Belkin granted departmental status in July 1961.
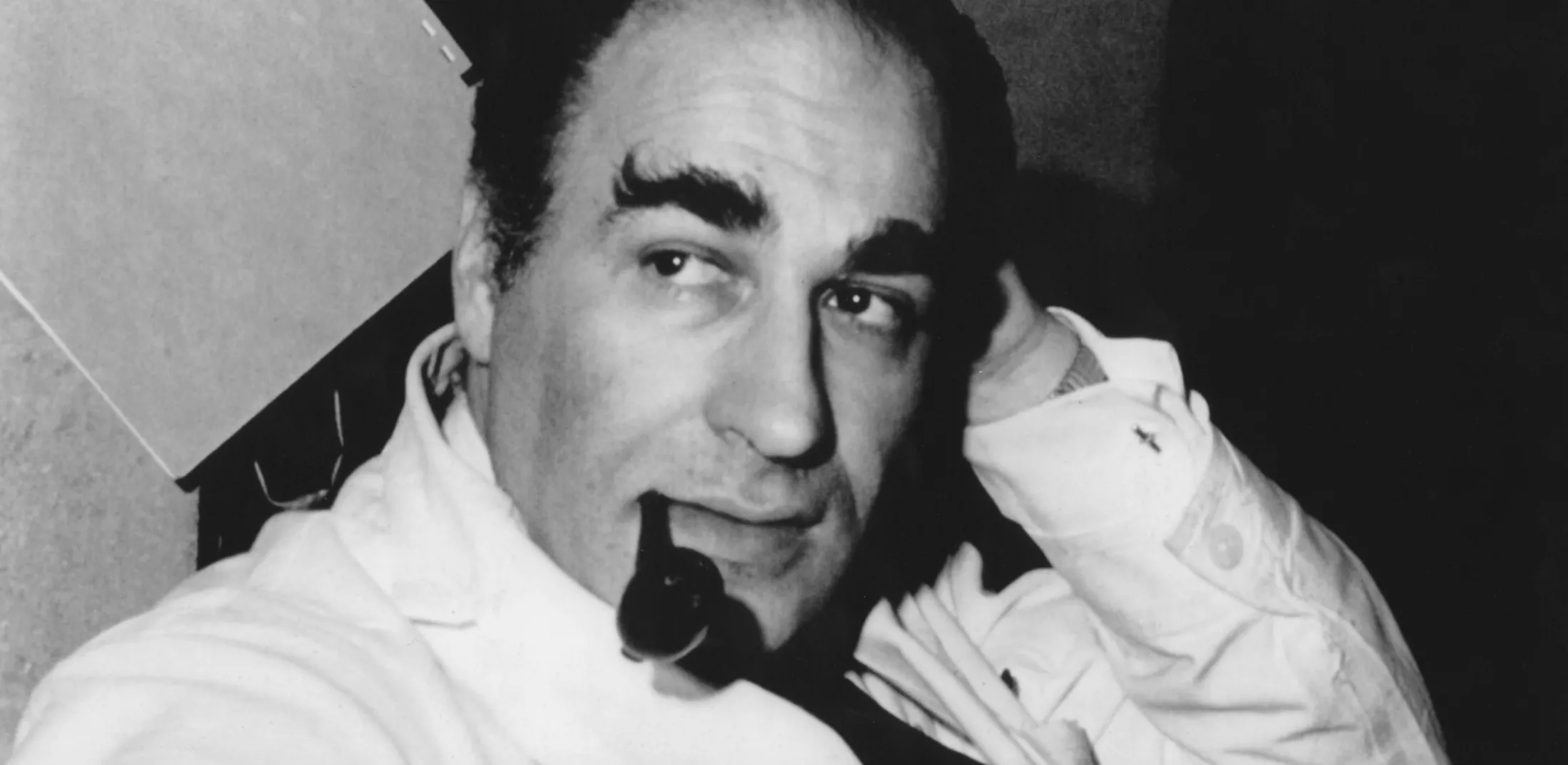
Dr. Saul R Korey: A Lasting Legacy
A Young Visionary
Saul R. Korey was 37 years old when in 1955 he left Case Western Reserve to come to the Bronx. Trained in neurology and neurochemistry, his vision was that neurologists/scientists should attempt to answer in the laboratory questions posed by patients, without sacrifice of humane and high quality clinical care. He sought out basic scientists like the organic chemists William Norton (1957) and Robert Ledeen (1962) as well as the biochemists Stanley Samuels (1960) and Amadeo D'Adamo (1963) to apply their knowledge of chemistry to the brain and human diseases. Also included in this eclectic group was Elliott Robbins (1960), who worked on mechanisms of mitosis, and Alan Finkelstein (1963), a membrane physiologist and a current Albert Einstein College of Medicine professor. As for the clinical faculty, Saul Korey did not ask us whether we would do research, he asked what research we intended to do. For example, Labe Scheinberg, who joined him in 1956, investigated immunological aspects of brain tumors and, later, multiple sclerosis. Labe Scheinberg was Saul Korey's right-hand clinical partner and faculty recruiter. Together with Louis Berlin, who died prematurely, and others, he trained generations of neurology residents. Labe Scheinberg was acting Chair and then Co-chair of the Department from 1963 to 1970 as well as Dean of the Medical School from 1970 to 1972. Robert Katzman, who came in 1957, first investigated electrolytes and water in the brain and then worked on Creutzfeldt-Jakob disease. He also joined Saul Korey and Kunihiko Suzuki in an early study of the neurochemistry of the Alzheimer brain, using the same biopsy material that led to the pioneering study of the ultrastructure of Alzheimer disease by Robert D. Terry, a neuropathologist recruited in 1959. At that time, Alzheimer's disease was considered to be presenile and thus rare, and dementia was thought to be an uninteresting though unfortunate aspect of normal aging.

Growing the Department
I was recruited in 1958, because I had training in child neurology, at the time a new aspect of neurology. Lawrence Taft, who joined the Department of Pediatrics in 1955, shared with me the running of child neurology service at Jacobi Hospital until 1973, when he left to become Chair of Pediatrics at Robert Wood Johnson Medical School. He was and is an expert in the care of handicapped children and was the founder of what became the Children's Evaluation and Rehabilitation Clinic (CERC). Saul Korey had invited Louis Costa, a quiet young neuropsychologist, starting a distinguished career, to carry out the behavioral studies he considered just as crucial to neurologic research as bench investigations. Influenced in part by Lou Costa, I started career-long clinical research on developmental disorders of communication, which brought me to a school for the deaf and to the study of autism and language disorders. Elliot Weitzman came in 1961, a fourth recruit from the residency at the Neurological Institute of Columbia Presbyterian Medical Center. He worked on neonatal electrophysiology and later on the relatively new field of sleep disorders and circadian rhythms. He died prematurely in 1983. Another early key figure was Molly Cox, sister of the future Solicitor General Archibald Cox, whom Labe Scheinberg brought from the electroencephalography (EEG) department of the Neurological Institute to organize a similar one at Jacobi Hospital. Although not a physician, she taught residents how to read EEGs for 28 years. Some residents, like Jerome (Pete) Engel and Solomon (Nico) Moshé, became international leaders in epilepsy and electrophysiology. Molly Cox served as the hub, mother confessor, and confidante of the entire Department until her retirement in 1985.
The Arrival of Dr. Oliver Sacks
A colorful early member of the Department, and surely by now its most widely known, was Oliver W. Sacks who arrived in 1965. He was attracted by the interdisciplinary vision of Saul Korey and by Bob Terry's research. After he found out that bench research was not for him, he moved to Beth Abraham Hospital where his weekly case conferences were the highlight of medical students' neurology rotations. His work in the Montefiore Headache Clinic provided the data for his first book, Migraine. When l-DOPA became available in 1967, he offered it to the profoundly affected post-encephalitic patients who had spent their lives in Beth Abraham Hospital since the post-World War I influenza pandemic. His startling observations of very rapid on-off effects,not seen in garden variety Parkinsonian patients but meticulously described in his 1973 book, Awakenings, were met with disbelief by neurologists. The changes in his patients were recorded in a documentary film created for British Television by Duncan Dallas (this is not the Hollywood romanticized movie of the same name starring Robin Williams as Oliver Sacks and Robert DeNiro as one of the patients). The neurologic community in the United States finally acknowledged the contribution of this work as well as his subsequent books in enhancing awareness of neurologic disability when both the American Academy of Neurology and the American Neurological Association accorded him prestigious lectureships. In the meanwhile, he had received a number of literary prizes and honorary degrees for his many other writings, including the 20 neurologic case histories in his best known book, The Man Who Mistook His Wife for a Hat.
The First—and Still the Best in the Country
Saul Korey organized the first neurobiologic Neurology Department in the country. Extraordinarily creative in his vision of science, he radiated enthusiasm and optimism, and he expected excellence as well as cross-departmental interdisciplinary collaboration from all members of the Department. He convinced the National Institute of Mental Health of the need for an interdisciplinary training program in the behavioral sciences. In its heyday, which lasted until the early 1970s, the interdisciplinary (ID) grant at Albert Einstein College of Medicine supported over two-dozen postdoctoral fellows in neuroscience, a few graduate students, allocated equal monies for faculty support and fellow stipends, and supported major symposia and seminars. I vividly remember symposia in the early 1960s on the size of the extracellular space in the brain, on the genetics of schizophrenia, and on lysosomes chaired by Dr. Alex Novikoff. Dr. Korey also applied to the National Institute of Neurological Diseases and Blindness (now the National Institute of Neurological Disorders and Stroke) for a Center grant, still active in its 37th year, which has supported creative research on a variety of neurodegenerative diseases (discussed later). These two grants played a key role in expanding the early faculty, including the recruitment of Dominick P. Purpura, our current Dean, to chair Anatomy and later Neuroscience. In addition, they provided the foundation for the enduring vigor of neuroscience research at Albert Einstein College of Medicine. As a distinguished laboratory investigator, Saul Korey was a driving force behind the building of the Ullmann tower, which more than doubled the medical school's research space. However, he did not live to see it completed.
An Ongoing Influence
It is a tribute to the strength of the early Department of Neurology that it kept its high morale and stayed largely intact for almost two decades after Dr. Korey's death from cancer at age 45. Saul Korey's vision was the glue that had kept us together through a period of turmoil and profound changes in medicine. He was a charismatic chairman and leader who backed his faculty and residents unconditionally in public, keeping criticisms private. A role model for all of us, he kept the door to his laboratory open to give us advice on difficult clinical cases, to vent new ideas, or discuss personal matters. He was utterly truthful, clear in what he saw as right, to his staff warm with a twinkle in his eye, yet he was viewed by those who knew him more casually as tough, uncompromising, and somewhat forbidding.
Adult Neurology: A World-Class Residency
The residency grew and shrank and grew again as Jacobi, Montefiore, and more recently Long Island Jewish, Beth Israel, and other hospitals became, ceased to be, or again became training sites. Robert Katzman was the Department's Chairman from 1964 until he moved to San Diego in 1984. He led the Department with evenhandedness and behind-the-scenes support. A quiet and reserved leader, he was always helpful but did not interfere with what was going well. His foresighted view of neurology as neurobiology enabled him to direct many enthusiastic and competent residents and post-residency fellows into fruitful lines of research. Several launched their academic careers at Albert Einstein College of Medicine before moving to other distinguished institutions. Among them were: Leonard J. Graziani studied neonatal neurology and went to Thomas Jefferson Medical School; Pete Engel studied epilepsy and EEG and went to the University of California at Los Angeles (UCLA); Bennett Shaywitz studied the biology of attention disorders and learning disabilities and went to Yale along with his wife Sally, an Albert Einstein College of Medicine-trained developmental pediatrician; S. David Holtzman studied the effects of anoxia on the neonatal brain and went to Stanford and later Harvard; Sakkubai Naidu studied metabolic disorders and went to Loyola and later to Johns Hopkins; Peter Dowling and Stuart Cook (who became Chairman of Neuroscience and in 1998 President of the University) studied neuroimmunology and went to the University of Medicine and Dentistry of New Jersey; Gary Rosenberg studied CSF dynamics and went to the University of New Mexico; Les Wolfson studied the extrapyramidal system and gait disorders and went to the University of Connecticut; and Leon Thal studied neuropharmacology and went to the University of California at San Diego. Andrew Doyle, a most promising member, died of cancer at age 37.
Pioneering Faculty
Herbert Schaumburg, another former resident, who also trained in neuropathology at Massachusetts General Hospital, succeeded Bob Katzman as Chairman. He, together with Peter Spencer, were pioneers in neurotoxicology. He was largely responsible, perhaps because of his expertise in peripheral neurology, for adding to the already strong EEG division neuromuscular electrophysiology. He faithfully attends weekly early morning neuromuscular rounds, the oldest clinical teaching conference in the Department, which was started by Labe Scheinberg in the 1960s. Herb Schaumburg was a driving force behind the close affiliation with Beth Israel's Neurology Department, where he trains residents to to care for patients with amyotrophic lateral sclerosis (ALS), movement disorders (under Susan Bressman's tutelage), and brain and spinal cord tumors (under the tutelage late Fred Epstein and Jeffrey Allen). Training in multiple sclerosis, which was an extremely active division of the East Campus (Jacobi/Weiler) under Murray Bornstein and Labe Scheinberg, is now provided at the St. Luke's-Roosevelt affiliate under Saud Sadiq.
By 2001, the Albert Einstein College of Medicine program had trained some 300 residents in neurology. A few of the outstanding clinical teachers were Labe Scheinberg and Denis Giblin at the East Campus, Jack Kessler, the popular chief of Neurology at Jacobi until 2000, as well as Michael Swerdlow and David Kaufman at Montefiore. Jack Kessler, who came to Albert Einstein College of Medicine in 1983, was director of the Kennedy Center from 1993 to 1998 and is now Chair of Neurology at Northwestern University. He is a distinguished investigator of growth factors and stem cells who attracted a number of young neurologists to the laboratory.
Decades of Notable Alumni
The Albert Einstein College of Medicine Neurology Department spawned clinicians who brought high quality neurologic practice to many parts of the country. The three tigers of the 1960s Stanley Mandell, Fidel Exconde, and David Rodvien, who were tragically killed in a car accident, competed in resident one-upmanship. A sampling of the high quality Albert Einstein College of Medicine-trained neurologists includes Robert Levine, Steven Jerett, John Lagios, Louis Cuzzone, Jan Mashman, Fidel Exconde, Leslie Wolfson, Reed Perron, Daniel Van Engel, Hugo Lijtmaer, Judith Lustig, Stanley Knep, and very recently Arun Kachroo. Arnold Sterman and Michael Gold work in research for drug companies. Judith Taylor, who became an early leader in the administration of health insurance and managed care programs, is now a historian living in northern California. John Whitaker, a neuroimmunologist who became Chairman of the Neurology Department at the University of Alabama in Birmingham, recently died prematurely of a head injury. Others who became Chairmen are Gary Rosenberg at the University of New Mexico in Albuquerque, Leon Thal at the University of California at San Diego, Les Wolfson at the University of Connecticut, Ronald Kanner at Long Island Jewish Hospital, Alan Berger at the University of Florida in Jacksonville, and Mark Mehler at Jacobi Medical Center and North Central Bronx Hospital.
Revolutionary Research
EEG, (encephalography,) which flourished under the influence of Pete Engel's clinical work and research on epilepsy, was greatly strengthened by the arrival in 1984 of Eli Goldensohn, whose retirement as Chief of Clinical Neurophysiology at the Neurological Institute was Albert Einstein College of Medicine's good fortune. He and Nico Moshé, who became Chief of the Electrophysiology Division in 1986, established the Albert Einstein College of Medicine training program in epileptology/ neurophysiology. Moshé's laboratory in the Kennedy Center investigates epileptogenesis and the turning off of seizures in the immature brain. Shlomo Shinnar, an Albert Einstein College of Medicine M.D./Ph.D. student whose mentor was Dom Purpura, came to us from Johns Hopkins University where he obtained his pediatric and pediatric neurology training. He and Nico Moshé developed the Montefiore epilepsy-monitoring unit and the epilepsy surgery program, a research and training site for the investigation of new drugs and refractory epilepsy in both children and adults. Harriet Kang and Karen Ballaban-Gil contribute to patient care, clinical research, and training in the Montefiore Epilepsy Unit. Allan Legatt, another home-grown M.D./Ph.D., is in charge of electrophysiologic monitoring of the brain and spinal cord during neurosurgical procedures and of clinical evoked potential testing at Montefiore.
Setting New Standards of Innovation
Building a Clinic for Headache Disorders
The Montefiore Einstein Headache Clinic was a legacy of Arnold Friedman from Columbia University who had established it in the 1950s. Later taken over by Seymour Solomon, the clinic was the New York Mecca for this common and incapacitating neurological condition. The epidemiologic studies of Richard Lipton have brought out that it is often poorly managed and costly in terms of days of work missed. Paul Winner, a former Albert Einstein College of Medicine child neurology fellow, has made similar observations about childhood headaches. Albert Einstein College of Medicine-trained neurologists with expertise in pain management include Russell Portnoy and Ron Kanner.
Pioneering Diagnoses for
Sleep Disorders
Elliott Weitzman developed the first sleep laboratory and was a pioneer in defining sleep apnea as a common and potentially serious medical problem. The sleep laboratory became in 1980 the fief of Michael Thorpy whose encyclopedic Handbook of Sleep Disorders is used worldwide. The pain and sleep units have trained a number of fellows and inspired many medical students and residents to enter these fascinating new fields of neurology.
The Department of Child Neurology
Creating a Globally Renowned Institution
The first child neurology trainee was Larry Schneck, who started in 1957 and read the entire Handbook of Neurophysiology while riding back and forth on the subway between Brooklyn and the Bronx. The division was supported by a National Institutes of Health (NIH) training grant during the 1960s until these grants were discontinued in the early 1970s. By now, 79 fellows have come through the program. As for Division Heads, Len Graziani (1964- 1968) was followed by Joseph H. French (1972-1979), a brilliant and charismatic clinician and neurochemist. Recruited to Albert Einstein College of Medicine in 1964, Dr. French studied mitochondrial respiration with Cyril Moore, who later became Chair of Biochemistry at Morehouse Medical School. Joe French was an expert on copper and other heavy metal metabolism in the brain. He was Director of the Children's Evaluation and Rehabilitation Center (CERC) from 1977 to 1978 and Assistant Dean for Student Education at Albert Einstein College of Medicine from 1970 to 1979. In 1980, he left Albert Einstein College of Medicine to join Henryk Wisniewski, another Albert Einstein College of Medicine transplant, at the New York State Institute for Basic Research in Mental Retardation and Director of Child Neurology at Downstate Medical School in Brooklyn. Joe died of cancer in 1999. Arthur Rose, trained in both child neurology and neuropathology and who investigated the effects of hyperbilirubinemia on the immature brain, succeeded him at Downstate.
Unparalleled Faculty
Alfred J. Spiro, an expert in neuromuscular diseases, joined the faculty in 1966. Al Spiro was Division Chief of Child Neurology at Albert Einstein College of Medicine from 1979 to 1995. Gerald S. Golden, was director of CERC from 1974 to 1977. He left to head Child Neurology in Galveston, then Memphis, and, in 1993, became Vice President of the National Board of Medical Examiners. Nico Moshé, currently Vice- Chair of the Department, came as fellow in 1975. In 1983, Shlomo Shinnar brought expertise in the epidemiology and long-term clinical course of epilepsy. Mitchell Steinschneider, another Albert Einstein College of Medicine M.D./Ph.D., who served his pediatric residency at Albert Einstein College of Medicine, was “loaned” to Columbia Presbyterian for his pediatric neurology fellowship, and was welcomed back as a valued teacher and an investigator of cortical auditory physiology in man and monkey.
A Global Influence
In 1970, Pongsakdi Visudhiphan single-handedly brought child neurology to Thailand, where it continues to thrive as a consequence of his Chairmanship at the Ramathibodi Hospital in Bangkok, and of his presidency of the Thai Child Neurology and Pediatric Societies. Kytjia Voeller became a world-renowned investigator of learning disorders and of the behavioral consequences of acquired right hemispheric lesions in children. Gerald Erenberg, expert in Tourette disease and academic disabilities, organized an efficient CERC at Morrisania Health Center. He moved to the Cleveland Clinic in 1975. Many practicing child neurologists, like Gerald Novack, Joseph Maytal, Trevor Resnick, and Roberto Tuchman continue to contribute to the literature. Also, former fellows Thaddeus Kurczynski in Ohio, Warren Cohen in Washington D. and Evelyn Traeger in New Jersey are now senior clinical geneticists/child neurologists. I was fortunate to be a founding member of both the Child Neurology Society and the International Child Neurology Association.
The Interdisciplinary Model
The Neurology Department has always worked closely with neurosurgery, neuroradiology, and neuropathology. For many years, the Friday morning Montefiore joint clinical conference chaired by Drs. Leo Davidoff of Neurosurgery, Harold Jacobson of Radiology, and Harry Zimmerman of Neuropathology was an important teaching conference for neurology residents and attending physicians. The arrival at Jacobi in 1960 of Mannie Schechter, a South African pioneer neuroradiologist trained in London to perform angiographies, myelographies, and pneumoencephalographies, marked a watershed in neuroradiology for this country. It was the start of interventional neuroradiology. Whereas Mannie Schechter's predecessors had read films while residents in neurology or neurosurgery performed these procedures, he and his trainees took them over in short order. When CT scanning became available in 1975, Robert Bernstein of Radiology procured a prototype model for Jacobi Hospital. Unfortunately, Mannie Schechter died prematurely from Alzheimer disease and did not see MRI revolutionize neuroimaging. Based on Mannie's early work, interventional neuroradiology at Montefiore has saved many patients with an aneurysm or arteriovenous malformation from the dangers and discomfort of open neurosurgical intervention.
Advancing Neuropathology
Neuropathology flourished at Albert Einstein College of Medicine, first under Harry Zimmerman, a world expert in brain tumors, then under his former trainee, Robert Terry. Bob Terry made major contributions, discussed later, to research on lysosomal diseases and, together with Henry Wisniewski and Dennis Dickson (his student), on the dementias. For years, neuropathology at Albert Einstein College of Medicine was the best and most productive department in the country. Asao Hirano at Montefiore trained close to a hundred young Japanese colleagues who have populated the academic neuropathology services of Japan. Asao worked on the ALS/parkinsonism/dementia complex of Guam, and the name Hirano bodies was assigned to the inclusions he described in the dementias. His exciting brain cutting conferences, the match of those of Bob Terry, Dikran Houroupian, and Dennis Dickson on the East campus, as well as the monthly muscle histopathology teaching conferences of Al Spiro, were critical elements in the training of neurology and neuropathology residents. It is indeed sad that the advent of managed care and fiscal accountability has shrunk clinical neuropathology to the vanishing point, despite the valiant efforts of its present Chief, Karen Weidenheim. High quality neurology cannot exist without neuropathology to verify difficult diagnoses and discover new diseases or new pathophysiologic concepts. The current weakness of academic neuropathology at Albert Einstein College of Medicine is a threat to the excellence of the Neurology Department, despite the outstanding contributions to be mentioned later of basic scientists like Peter Davies, Cedric Raine, and Celia Brosnan.
On the Cutting Edge of Neurochemistry
In 1986, Kuni Suzuki, who had trained in neurochemistry with Saul Korey, moved to Chapel Hill Medical School to head their Neuroscience Center. Together with his neuropathologist wife and collaborator, Kinuko Suzuki, he made important contributions to the understanding of other lysosomal diseases. The focus of some of his work was the enzymatic deficiency and, later, the molecular basis of Krabbe disease, a leukodystrophy of infancy which destroys the brain rather than causing the massive neuronal storage of Tay-Sachs disease. More than a quarter century ago Kuni proposed that the cause of neuronal death in this disease and in infantile Gaucher disease was the accumulation of toxic galacto- and glucosphingosine, intermediaries in alternate catabolic pathways resulting from the enzymatic block. New variants of GM1 and GM2 gangliosidosis, sialidosis, and other storage diseases were discovered by meticulous neuropathologic and neurochemical collaborative investigations in neurologically well-studied patients. Steve Walkley's current research on prevention or reversal by transplantation, into feline models of storage diseases, stands on the shoulders of this early work.
Neurochemistry: Interdisciplinary Research Highlights
Besides myelin studies, Norton's laboratory engaged in other interdisciplinary studies: James Goldman, now Chief of Neuropathology at Columbia, Alex Chiu, now in Bob Yu's Institute at the Medical College of Georgia, and Dennis Aquino, now at Schering-Plough, investigated brain intermediate filaments. Jose Amat, now a psychiatrist, was concerned with cell proliferation following brain injury. These colleagues, and dozens of graduate students and postdoctoral fellows in neuroscience trained by neurology and neuropathology faculty, have taken positions in other medical schools around the country or in industry, bringing with them the collaborative interdisciplinary outlook they had acquired from the Korey/Terry/Norton laboratories.
Breakthrough Progress for Alzheimer’s Treatment
In 1963, following up on the approach pioneered by Saul Korey, Bob Terry applied the newly maturing technique of electron microscopy to human biopsy tissue; he identified the ultrastructural pathology of Alzheimer disease, the amyloid plaque and paired helical filament, findings that opened the way to studies of the neurobiology of this disorder. In 1988, Bob Terry was awarded the first Potamkin Prize for Research on Alzheimer Disease, an honor given by the American Academy of Neurology. Kuni Suzuki and Bob Katzman completed an analysis of the neurochemical changes in biopsies initiated by Saul Korey. Bob Terry recruited a team of neuropathologists that included Nicholas Gonatas (who married Jackie Orloff, Saul Korey's technician), Henry Wisniewski, Michael Shelanski, Peter Davies, Khalid Iqbal, Inge GrundkeIqbal, and Dennis Dickson, who continued to advance the field. Peter Werner, who studies molecular mechanisms of neurodegenerative diseases, is the newest investigator in this area. Identification of amyloid in plaques, and of paired helical filaments and tau protein mutations in the neuronal tangles of Alzheimer's disease, Pick disease, and other dementing conditions were some of the fruits of this wide ranging interdisciplinary research program. Peter Davies' discovery of the cholinergic deficiency in Alzheimer brains was the basis for clinical trials of cholinesterase antagonists and cholinergic replacement therapy by Leon Thal. Later, Leon Thal left with Bob Katzman and Bob Terry for San Diego; there he conducted large treatment studies that led to the only Food and Drug Administration (FDA)-approved specific pharmacologic treatment for Alzheimer disease.
The Bronx Aging Study
Initial clinical-pathological studies, which had begun with the efforts of Bob Katzman, Jay Coblentz, Hugo Lijtmaer, Paula Fuld, and Wilma Rosen in advanced dementia cases at the Jewish Home and Hospital, evolved into a major longitudinal study of aging in normal elderly: The Bronx Aging Study. This prospective study was organized with help of Miriam Aronson, a gerontologist with a primary appointment in the Department of Psychiatry. The study was multidisciplinary, involving neuropathology, neurology, neuropsychology, and statistics (including collaborations with Herbert Schimmel and Ted Brown of Queens College). Among the participating neurologists were Herman Buschke, Les Wolfson, and Howard Crystal. Howard Crystal later took over the related Teaching Nursing Home project; he recently left Albert Einstein College of Medicine for Downstate. In the Bronx Aging Study, neuropsychologic, neurological, and medical tests were meticulously carried out in a cohort of elderly residents who volunteered to donate their brains after their demise. This enabled studies of the incidence, course and symptomatology of late life dementia. Further, it enabled the differentiation of benign forgetfulness from progressive memory deterioration on the basis of memory tests developed earlier by Herman Buschke, Steve Mattis, Paula Fuld, and their collaborators. The study was not limited to neurologic studies of normal and pathologic aging, as it provided William Frishman of the Department of Medicine the opportunity to follow cardiovascular pathology in late life.
NIH-Supported Progress
Following the success of l-Dopa (and a sabbatical at the University of Lund with Anders Bjorklund), Bob Katzman was able to obtain NIH support that permitted Leon Thal to collaborate with Maynard Makman of the Department of Biochemistry on the investigation of dopamine receptors, and to recruit as postdoctoral fellows Richard Meibach (now at Roche), Sander Glatt (now at Kansas University Medical Center), and Lucy Brown. Lucy Brown, now professor of Neurology and Neuroscience, is concerned with the neurobiology of movement disorders. She and Les Wolfson, using deoxyglucose autoradiography, defined regions of activation in the striatum and subthalamic nucleus after dopamine administration in animals. Lucy Brown expanded this work to describe functional neuroanatomic organization of sensorimotor activity in the basal ganglia as a grid or lattice-like structure. She is now collaborating in functional MRI studies of the basal ganglia in both animals and man.
Advanced Treatment Trials for Peroxisomal Diseases
While he was at the Massachusetts General Hospital, Herb Schaumburg started the study of a series of cases of adrenoleukodystrophy in which he and Jim Powers, an Albert Einstein College of Medicine trainee in neuropathology, described thin leaflet within the adrenal gland, testis, Schwann cells, and oligodendroglia. Together with Kuni Suzuki, his trainee M. Igarashi, and others they discovered the accumulation of very long chain fatty acids that characterizes this disease and other peroxisomal diseases. Their findings led Ann and Hugo Moser and their collaborators at Johns Hopkins University to the discovery of the missing enzyme, cloning of the gene, genetic testing, and treatment trials for this lethal disease of adolescent boys.
The most exciting seminar of my career focused on the interdisciplinary study of two floppy, severely retarded, marasmic infants with seizures who had died of a then obscure lethal genetic condition, Zellweger disease. At this conference Sidney Goldfisher, an expert on the liver, reported his inability to detect any of the normally abundant peroxisomes in the liver. Peroxisomes were not to be found in the kidney tubules either. Mitochondrial function was impaired as well, as Cyril Moore had uncovered defective respiration in isolated mitochondria from brain and liver biopsies, confirmed by the histochemical observations of the neuropathologist Anne Johnson, and by distorted mitochondrial architecture in all the organs sampled. Study of these two infants provided the kickstart to unraveling the pathobiology of this and other peroxisomal diseases, including another infant with a similar clinical picture whose peroxisomes were present but inactive due to a single missing enzyme. The Moser laboratory went on to propose a rational classification of peroxisomal diseases affecting children with what had been until then disparate genetic disorders.
Breakthrough Progress in Understanding Multiple Sclerosis
Multiple sclerosis (MS) is the most frequent devastating neurologic disease of young adults. Murray Bornstein, a neurologist recruited from the Neurological Institute in 1966, brought to the Department the expertise in organotypic tissue culture of Edith Peterson. The tissue culture laboratory of the Kennedy Center became the indispensable tool for many basic science investigators. Murray Bornstein, who died unexpectedly in 1995, was the force behind investigation of copolymer as a protective treatment for the exacerbations of multiple sclerosis, one of two drugs now approved by the FDA. Labe Scheinberg's interdisciplinary comprehensive MS center showed residents that one could always do something helpful for chronically disabled patients, even when one cannot cure their disease. Other studies of MS included ultrastructural observations of biopsied plaques by Kinuko Suzuki and Bob Terry. The tissue they used was from patients who were undergoing neurosurgical interventions by Irving Cooper at St. Barnabas Hospital to improve their ataxia. They also make a large series of studies in the animal model for MS, experimental allergic encephalomyelitis. Stuart Cook, Peter Dowling, and John Prineas, an Australian, took off from their Albert Einstein College of Medicine residencies to Newark, and the late John Whitaker who went to the University of Alabama at Birmingham, have carried on career-long investigations of the immunologic basis of MS, disseminated encephalomyelitis, and acute autoimmune polyneuritis.
A Cross-Disciplinary Team of Experts
Saul Korey's longstanding interest in brain lipids, myelin and demyelination motivated Bill Norton's fundamental investigations of lipid structure, done in collaboration with Maurice Rapport, now a retired senior neuroscientist and visiting professor in our Department. Bill Norton and his colleagues Lucy Autilio Gambetti and Shirley Poduslo devised isolation methods for myelin and intact viable CNS cells, and Wendy Cammer investigated myelin enzymes and mechanisms of oligodendrocyte death. She and Cyril Moore discovered in 1972 that the liquid cleanser Phisohex, up to then widely used in newborn nurseries, was toxic to mitochondria and resulted in myelin edema. Kay Fields, now at the NIH, studied immunocytochemistry of brain-specific antigens and Jorge Larocca is concerned with receptors and signal transduction in oligodendroglia. Cedric Raine, recruited to Neuropathology by Bob Terry in 1976, and Celia Brosnan, at Albert Einstein College of Medicine since 1968, have investigated the inflammatory cascade that culminates in the demyelinated MS plaques, and are now working to unravel the genes and their products responsible for this pathology.
Leading-Edge Stem Cell Research
Jack Kessler, who came to Albert Einstein College of Medicine from the Cornell neurology service in 1983, brought with him the rigorous approach to clinical neurologic problems he acquired from his mentor, Fred Plum. His research focused on stem cells and the effects of growth factors on neurologic development, disease, and repair. Bright Albert Einstein College of Medicine-trained neurologists, among them Stuart Apfel who studied the effect of nerve growth factor in diabetic neuropathy, Daniel Rosenbaum concerned with neuroprotection for the prevention of cell death in the penumbra of strokes, Peter Mabie who works on the mechanisms of central nervous system progenitor cell differentiation, and others joined the Kessler laboratory in the Kennedy Center. In 2000, Jack Kessler left to become the Chair of Neurology at Northwestern Medical School. At present, Mark Mehler, an expert in cognitive disorders and molecular biology, in collaboration with other vigorous young Kennedy neurologists/investigators, is expanding research in stem cell and cytokine biology. They also are working to develop novel therapeutic strategies for intractable neurodegenerative diseases like Alzheimer's and Huntington's diseases.
Accelerating a Deeper Understanding of Epilepsy
Herb Vaughan's laboratory in the Kennedy Center has over the years been concerned with the sources of various components of event-related potentials during sensory stimulation and language in both children and adults. Current collaborative research of Michelle Dunn, a pediatric neuropsychologist and electrophysiologist, and Judith Gravel, a pediatric audiologist, is addressing systematically the physiologic basis of the auditory and language deficits of children on the autistic spectrum. Herb Vaughan, Diane Kurtzberg (his wife), Walter Ritter, Joseph Arezzo, and many other Kennedy Center collaborators from the Neuroscience Department have carried out systematic studies mapping the development of cortical auditory and visual event-related potentials in monkeys, premature infants, term infants, and children with chronic otitis media and other handicaps. They also studied normal adults and those with various brain pathologies. A major early contribution of the Vaughan laboratory was the demonstration that the source of early auditory event-related potentials, best recorded at the vertex, originated in the primary auditory cortex. The laboratory trained dozens of electrophysiologists. Among them are Alan Legatt, who records intraoperative studies, and Mitch Steinschneider, who has succeeded in recording, in monkeys and in patients under-going surgery for the control of epilepsy, the physiologic correlates of the processing of voiced and unvoiced consonant sounds.
Nico Moshé and collaborators were the first to induce kindling in the immature rat; they also demonstrated the influence of sex hormones and age on the substantia nigra's role in the control of seizures. They have been investigating increased seizure susceptibility and rapid transition from partial to generalized seizures in the immature rat brain. These studies parallel the clinical studies of Shlomo Shinnar who examined the functional consequences of febrile seizures and status epilepticus as well as the long-term outcome of patients with single seizures, uncomplicated seizures, and epilepsy in patients with structural brain lesions.
A Best-In-Class Neurology Department
Cultivating Excellence from the Start
The strong research contribution of the Neurology Department is unique and directly attributable to Saul Korey's emphasis on interdisciplinary collaboration. This strength encouraged Dom Purpura, at the time Chair of Anatomy and Director of the Kennedy Center, to convince the Dean and Trustees of the need to create a now flourishing Department of Neuroscience. Most of the neurology faculty that carry out basic science research had dual appointments in Neurology and Neuroscience. The contributions to the literature of the present and former members of the Neurology Department are extremely large in number and span almost every aspect of clinical neurology as well as applied and basic neurologic research. Their contributions have been recognized nationally and internationally by their appointment to NIH study sections and councils of the National Institute of Neurological Diseases and Stroke and the National Institute of Aging. Several have become officers of the major neurologic societies (Bob Katzman was president of the American Neurological Association in 1986-1987, John Whitaker in 1996-1998), many as members of their standing committees. Both Bill Norton and Kuni Suzuki were presidents of the American Society for Neurochemistry and Chief Editors of the Journal of Neurochemistry; Robert Yu is currently president elect of the American Society for Neurochemistry; and Cedric Raine is founding editor of the Journal of Neuroimmunology. Pete Engel was president of the American Epilepsy Society, the American Clinical Neurophysiology Society and the International League Against Epilepsy. Nico Moshé is currently the president of the American Epilepsy Society and served as president of the American Clinical Neurophysiology Society. Many members of the Department have served on boards of volunteer granting agencies, have received prizes, and been invited to lecture worldwide and deliver prestigious named lectureships. A number of Albert Einstein College of Medicine medical students have chosen careers in adult or child neurology elsewhere in the country and several leading medical schools have adopted Saul Korey's vision of neurology as a branch of neurobiology. His name is perpetuated at the annual meeting of the American Academy of Neurology by the Saul R. Korey Award for an essay on experimental neurology submitted by a medical student, and by the annual Saul R. Korey Lecture at the meeting of the Neuropathological Society. A lasting contribution of the Saul R. Korey Department of Neurology to Albert Einstein College of Medicine is the demonstration that collaboration pays off in science, and that a broad vision of clinical and basic science can lead very far.