Women’s Heart Disease
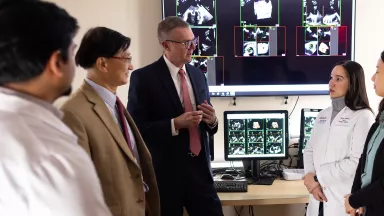
At the Montefiore Einstein Center for Heart and Vascular Care, you can access exceptional care for women’s heart disease. As a global leader in cardiovascular medicine and surgery, we are an academic-based, national and international referral site for high-risk and complex cases. For more than a century, we have been at the forefront in treating heart disease.
Ranked in the top one percent of all hospitals in the nation for Cardiology, Heart & Vascular Surgery according to U.S. News & World Report, our specialists are passionate about uncovering the latest diagnostic approaches and treatments that can improve outcomes. Backed by a multidisciplinary team of specialists, Montefiore Einstein continues to make advances in the treatment of heart disease. In recent years, we have expanded our programs in advanced cardiac imaging, heart failure and interventional cardiovascular medicine and assembled a world-renowned cardiothoracic surgical team.
When you trust us with your care, you can expect compassionate, personalized treatment plans that meet the highest standards for quality and safety. In addition, we offer patients a full choice of support services, from nutritional guidance to rehabilitative therapies.
When you need care for women’s heart disease, turn to our dedicated providers who will develop a highly personalized treatment plan specific to you.
As part of an academic health system, Montefiore Einstein Center for Heart and Vascular Care supports the mission and guidelines of the U.S. Department of Health and Human Services (HHS). The following information is provided by HHS.
Coronary Heart Disease - Women and Heart Disease
Coronary heart disease is the leading cause of death for women. About 80% of women ages 40 to 60 have one or more risk factors for coronary heart disease. Having multiple risk factors significantly increases a woman’s chance of developing coronary heart disease.
Learn more about how the causes, risk factors, symptoms, diagnosis, and treatment of coronary heart disease may be different for women than for men. Read Advancing Women's Heart Health to learn more.
Why does coronary heart disease affect women differently?
Coronary heart disease is different for women than men because of hormonal and anatomical differences.
- Hormonal changes affect a woman’s risk for coronary heart disease. Before menopause, the hormone estrogen provides women with some protection against coronary artery disease. Estrogen raises levels of HDL cholesterol (sometimes called “good” cholesterol) and helps keep the arteries flexible so they can widen to deliver more oxygen to the tissues of the heart in response to chemical and electrical signals. After menopause, estrogen levels drop, increasing a woman’s risk for coronary heart disease.
- The size and structure of the heart is different for women and men. A woman’s heart and blood vessels are smaller, and the muscular walls of women’s hearts are thinner.
- Women are more likely to have nonobstructive coronary heart disease or coronary microvascular disease. These types are harder to diagnose than obstructive coronary artery disease, which can be harder to diagnose. This can cause delays in getting diagnosed and treated.
What factors affect risk for women differently?
Coronary Heart Disease - Women are more likely than men to have medical conditions or life issues that raise their risk for coronary heart disease.
- Anemia, especially during pregnancy
- Early menopause (before age 40)
- Endometriosis
- High blood pressure after age 65
- History of problems during pregnancy, including gestational diabetes, preeclampsia, eclampsia (high blood pressure during pregnancy), and giving birth to a baby who is premature or smaller than average.
- Hormonal birth control
- Inflammatory and autoimmune diseases
- Lack of physical activity
- Mental health issues, such as stress, marital stress, anxiety, depression, or low social support
- Metabolic syndrome, a group of risk factors that raises your risk of heart disease and other health problems
- Overweight and obesity
Some factors raise women’s risk for coronary heart disease more than they increase risk in men.
- Diabetes
- Low levels of HDL cholesterol
- Mild to moderate high blood pressure
- Smoking
Visit The Heart Truth® to learn more about coronary heart disease risk factors for women and how to lower them.
Can symptoms differ for women?
Although men and women can experience the same symptoms of coronary heart disease, women often experience no symptoms or have different symptoms than men do.
- Activity that brings on chest pain. In men, angina tends to worsen with physical activity and go away with rest. Women are more likely than men to have angina while they are resting. In women who have coronary microvascular disease, angina often happens during routine daily activities, such as shopping or cooking, rather than during exercise. Microvascular angina events may last longer and be more painful than other types of angina.
- Location and type of pain. Pain symptoms are different for each person. Women having angina or a heart attack often describe their chest pain as crushing, or they say it feels like pressure, squeezing, or tightness. Women may have pain in the chest or the neck and throat.
- Mental stress. Mental stress is more likely to trigger angina pain in women than in men.
- Other symptoms. Common signs and symptoms for women include nausea, vomiting, shortness of breath, abdominal pain, sleep problems, Fatigue, and lack of energy.
What do women need to know about diagnosis and treatment?
Tests and procedures for diagnosing coronary heart disease are very similar for women and men. But women may experience delays in diagnosis or treatment. Learn about important diagnostic tests and treatment options.
- Ask about important diagnostic tests. Doctors are less likely to refer women for diagnostic tests for coronary heart disease. When women go to the hospital for heart symptoms, they are more likely than men to experience delays receiving an initial EKG, are less likely to receive care from a heart specialist during hospitalization, and are less likely to receive certain types of therapy and medicines. Younger women are more likely than men to be misdiagnosed and sent home from the emergency department after cardiac events that occur from undiagnosed and untreated vascular heart disease.
- Ask about treatment options that are effective for men and women. Women may be less likely than men to receive aspirin, statins, and beta blockers for treating their heart disease. Although women may be as likely as men to benefit from a pacemaker or a defibrillator, women are less likely to receive these treatments for complications of coronary heart disease. Women are often less likely to receive percutaneous coronary intervention or coronary artery bypass grafting than men are, even though research shows that both men and women can benefit from these procedures.
- Know and share your risk factors. Doctors may not recognize women’s risk for coronary heart disease. Commonly used risk-scoring systems may not accurately predict risk in women. Also, in one survey, fewer than one in four women reported that their doctors had ever discussed their risk for heart disease.
- Learn the symptoms and seek medical care right away. Being familiar with the symptoms of coronary heart disease and how they may differ in women may help you recognize when to talk to your doctor or when to seek medical care. Immediate care may help prevent complications such as heart attack or sudden cardiac arrest.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/86297
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2019-01-22 15:53:00.0