Heart Failure & Cardiomyopathies
At the Montefiore Einstein Center for Heart and Vascular Care, you can access exceptional care for heart failure and cardiomyopathies. As a global leader in cardiovascular medicine and surgery, we are an academic-based, national and international referral site for high-risk and complex cases. For more than a century, we have been at the forefront in treating heart disease.
Ranked in the top one percent of all hospitals in the nation for Cardiology, Heart & Vascular Surgery according to U.S. News & World Report, our specialists are passionate about uncovering the latest diagnostic approaches and treatments that can improve outcomes. Backed by a multidisciplinary team of specialists, Montefiore Einstein continues to make advances in the treatment of heart disease. In recent years, we have expanded our programs in advanced cardiac imaging, heart failure and interventional cardiovascular medicine and assembled a world-renowned cardiothoracic surgical team.
When you trust us with your care, you can expect compassionate, personalized treatment plans that meet the highest standards for quality and safety. In addition, we offer patients a full choice of support services, from nutritional guidance to rehabilitative therapies.
When you need care for heart failure and cardiomyopathy, turn to our dedicated providers who will develop a highly personalized treatment plan specific to you.
As part of an academic health system, Montefiore Einstein Center for Heart and Vascular Care supports the mission and guidelines of the U.S. Department of Health and Human Services (HHS). The following information is provided by HHS.
Heart Failure Treatment
Heart failure has no cure. But treatment can help you live a longer, more active life with fewer symptoms. Treatment depends on the type of heart failure you have and how serious it is but usually includes heart-healthy lifestyle changes and medicines. You may need a procedure or surgery for some types of serious heart failure. Because heart failure often gets worse over time, it is important for you and your caregivers to discuss your long-term treatment goals with your healthcare team.
Your healthcare team will also treat any medical condition that caused or worsens your heart failure.
This video describes possible treatments for heart failure, including lifestyle changes, medicines such as diuretics to get rid of excess fluid, or a heart procedure or surgery. Medical Animation Copyright © 2021 Nucleus Medical Media Inc. All rights reserved.
Your healthcare team may include a cardiologist (a doctor who specializes in treating heart conditions), nurses, your primary care doctor, pharmacists, a dietitian, physical therapists and other members of your cardiac rehabilitation team, and social workers.
Healthy Lifestyle Changes
Your doctor may recommend these heart-healthy lifestyle changes alone or as part of a cardiac rehabilitation plan:
- Lower your sodium (salt) intake. Salt may make your fluid buildup worse. View our Tips To Reduce Salt and Sodium fact sheet.
- Aim for a healthy weight since extra weight can make your heart work harder.
- Get regular physical activity. Ask your doctor about how active you should be, including during daily activities, work, leisure time, sex, and exercise. Your level of activity will depend on how serious your heart failure is. Sometimes, your healthcare provider might recommend outpatient cardiac rehabilitation services to improve what level of exercise you can do and reduce your risk factors.
- Quit smoking. View Smoking and Your Heart for more information. For free help quitting smoking, you may call the National Cancer Institute’s Smoking Quitline at 1-877-44U-QUIT (1-877-448-7848).
- Avoid or limit alcohol. Your doctor may recommend that you limit or stop drinking alcohol. You can find resources and support at the National Institute on Alcohol Abuse and Alcoholism’s Alcohol Treatment Navigator.
- Manage contributing risk factors. Controlling some of the factors that may worsen heart failure like blood pressure, heart rhythm, and anemia will often improve heart health.
- Manage stress. Learning how to manage stress and cope with problems can improve your mental and physical health. Learning relaxation techniques, talking to a counselor, and finding a support group can all help. Visit Relaxation Techniques for Health to learn more about how relaxation techniques can help lower stress and anxiety.
- Get good-quality sleep. Sleep disorders such as sleep apnea are common in people who have heart failure. Treating your sleep disorder helps improve your sleep and may help improve your heart failure symptoms.
Learn more about these healthy lifestyle changes in our Heart-Healthy Living Health Topic.
Medicines
Your doctor may prescribe medicines based on the type of heart failure you have, how serious it is, and your response to certain medicines.
Left-sided heart failure
The following medicines are commonly used to treat heart failure with reduced ejection fraction.
- Medicines to remove extra sodium and fluid from your body, including diuretics and aldosterone antagonists (such as spironolactone). These medicines lower the amount of blood that the heart must pump. Very high doses of diuretics may cause low blood pressure, kidney disease, and worsening heart failure symptoms. Side effects of aldosterone antagonists can include kidney disease and high potassium levels.
- Medicine to relax your blood vessels to make it easier for your heart to pump blood. Examples include angiotensin converting enzyme inhibitors and angiotensin receptor blockers. Possible side effects include cough, low blood pressure, and short-term reduced kidney function.
- Medicines to slow your heart rate, such as beta blockers and ivabradine. These medicines make it easier for your heart to pump blood and can help prevent long-term heart failure from getting worse. Possible side effects include a slow or irregular heart rate, high blood pressure, and fuzzy vision or seeing bright halos.
- Newer medications. Two new groups of medicines approved to lower blood sugar in patients with diabetes, sodium-glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide (GLP) agonists, may also reduce heart failure hospitalizations. Their use in treating heart failure is currently being studied.
- Digoxin to make your heart beat stronger and pump more blood. This medicine is mostly used to treat serious heart failure when other medicines do not help improve your symptoms. Side effects may include digestive problems, confusion, and vision problems.
Currently, the main treatment for heart failure with preserved ejection fraction are diuretics. Your doctor also may prescribe blood pressure medicines to help relieve your symptoms.
Right-sided heart failure
If you have right-sided heart failure, your doctor may prescribe medicines to remove extra sodium and fluid from your body, and medicines to relax your blood vessels.
Procedures & Surgeries
If your heart failure with reduced ejection fraction worsens, you may need one of the following medical devices:
- A biventricular pacemaker (also called cardiac resynchronization therapy). This can help both sides of your heart contract at the same time to relieve your symptoms.
- A mechanical heart pump, such as a ventricular assist device or a total artificial heart. You may use a heart pump until you have surgery or as a long-term treatment.
- An implantable cardioverter defibrillator (ICD). An ICD checks your heart rate and uses electrical pulses to correct irregular heart rhythms that can cause sudden cardiac arrest.
You may also need heart surgery to repair a congenital heart defect or damage to your heart. If your heart failure is life-threatening and other treatments have not worked, you may need a heart transplant.
For people with heart failure and preserved ejection fraction, there are no currently approved devices or procedures to improve symptoms. Researchers are continuing to study possible treatments.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4375
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-28 20:09:00.0
Heart Failure Diagnosis
Your doctor will diagnose heart failure based on your medical history, a physical exam, and test results. Your doctor may also refer you to a cardiologist for these tests and treatment. A cardiologist is a doctor who specializes in diagnosing and treating heart diseases.
Medical History & Physical Exam
Bring a list of your symptoms to your doctor’s appointment, including how often they happen and when they started. Also, bring a list of any prescription and over-the-counter medicines you take. Let your doctor know if you have any risk factors for heart failure.
During your physical exam, your doctor will:
- Measure your heart rate, blood pressure, and body weight.
- Listen to your heart with a stethoscope for sounds that suggest that your heart is not working properly.
- Listen to your lungs for the sounds of fluid buildup.
- Look for swelling in your ankles, feet, legs, liver, and veins in your neck.
Diagnostic Tests & Procedures
This animation discusses some of the tests used to diagnose heart failure. These tests may include an electrocardiogram to look at your heart’s electrical activity, an echocardiogram to measure how well your heart is working and look at the structure, and a chest X-ray to see if your heart is enlarged or there is fluid in your lungs. Other tests may include blood tests and an exercise, or stress test. Medical Animation Copyright © 2021 Nucleus Medical Media Inc. All rights reserved.
Blood tests
Your doctor may order blood tests to check the levels of certain molecules, such as brain natriuretic peptide (BNP). These levels rise during heart failure. Blood tests can also show how well your liver and your kidneys are working.
Tests to measure your ejection fraction
Your doctor may order an echocardiography (echo) or other imaging tests to measure your ejection fraction. Your ejection fraction is the percent of the blood in the lower left chamber of your heart (the left ventricle) that is pumped out of your heart with each heartbeat. Ejection fraction tells your doctor how well your heart pumps. This helps your doctor diagnose the type of heart failure you have and guide your treatment.
- If 40% or less of the blood in your left ventricle is pumped out in one beat, you have heart failure with reduced ejection fraction.
- If 50% or more of the blood in your left ventricle is pumped out in one beat, you have heart failure with preserved ejection fraction.
If your ejection fraction is somewhere in between (41% to 49%), you may be diagnosed with heart failure with borderline ejection fraction.
Other tests
- Other imaging tests to show how well your heart is working, such as a cardiac CT scan, cardiac MRI, or nuclear heart scan. To look inside the arteries in your heart to see if they are blocked, you may also need cardiac catheterization with coronary angiography.
- Tests for your heart’s electrical activity, including an electrocardiogram (EKG) or a Holter or event monitor that you wear for 24 to 48 hours or longer while going about your normal activities.
- A stress test to measure how much exercise your body can handle and how well it works during physical activity. Some heart problems are easier to diagnose when your heart is working hard and beating fast.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4374
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-16 14:03:00.0
Heart Failure Causes
Chronic (long-term) heart failure is often caused by other medical conditions that damage or overwork your heart. Acute (sudden) heart failure can be caused by an injury or infection that damages your heart, a heart attack, or a blood clot in your lung.
To understand heart failure, it helps to know how the heart works. The right side of your heart gets oxygen-low blood from your body. It pumps the blood to your lungs to pick up oxygen. The left side of your heart pumps oxygen-rich blood to the rest of your body.
This animation describes heart failure and some of its causes. Medical Animation Copyright © 2021 Nucleus Medical Media Inc. All rights reserved.
What Causes Left-Sided Heart Failure?
Left-sided heart failure is more common than right-sided heart failure. There are two types of left-sided heart failure, each based on how well your heart can pump. This measurement is called the ejection fraction. Visit the Diagnosis section to learn more about the ejection fraction.
- In heart failure with reduced ejection fraction (HFrEF), the left side of your heart is weak and can’t pump enough blood to the rest of your body. Chronic (long-term) conditions that damage or weaken the heart muscle are the main cause of heart failure with reduced ejection fraction. For example, coronary heart disease or a heart attack can prevent your heart muscle from getting enough oxygen (shown below). Other causes of this type of heart failure include faulty heart valves, an irregular heartbeat, or heart diseases that you are born with or inherit.
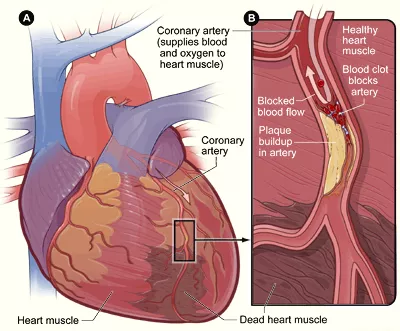
How a heart attack can lead to heart failure. Figure A shows dead heart muscle caused by a heart attack. Figure B is a close-up showing how a blocked artery in the heart prevents the heart muscle from getting oxygen. The heart muscle begins to die, weakening the heart
- In heart failure with preserved ejection fraction (HFpEF), the left side of your heart is too stiff to fully relax between heartbeats. That means it can't fill up with enough blood to pump out to your body. High blood pressure and other conditions that make your heart work harder are the main causes of heart failure with preserved ejection fraction. Conditions that stiffen the chambers of the heart such as obesity and diabetes are also causes of this type of heart failure. Over time, your heart muscle thickens to adapt, which makes it stiffer.
Visit the Diagnosis section to learn more about heart failure with preserved or reduced ejection fraction and how doctors diagnose it.
What Causes Right-Sided Heart Failure?
Over time left-sided heart failure can lead to right-sided heart failure.
In right-sided heart failure, your heart can't pump enough blood to your lungs to pick up oxygen. Left-sided heart failure is the main cause of right-sided heart failure. That’s because left-sided heart failure can cause blood to build up on the left side of your heart. The build-up of blood raises the pressure in the blood vessels that carry blood from your heart to your lungs. This is called pulmonary hypertension, and it can make the right side of your heart work harder.
Congenital heart defects or conditions that damage the right side of your heart such as abnormal heart valves can also lead to right-side heart failure on its own. The same is true for conditions that damage the lungs, such as chronic obstructive pulmonary disease (COPD).
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4371
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-16 13:58:00.0
Heart Failure Risk Factors
Many factors can raise your risk of heart failure. Some factors you can control, such as lifestyle habits. Others you cannot, including your age, race, or ethnicity. Your risk of heart failure goes up if you have more than one of these factors.
- Age. People 65 years or older have a higher risk of heart failure because aging can weaken and stiffen your heart. Older adults are also more likely to have other health conditions that cause heart failure.
- Family history and genetics. Your risk of heart failure is higher if people in your family have been diagnosed with heart failure. Certain gene mutations can also raise your risk. These mutations make your heart tissue weaker or less flexible.
- Lifestyle habits. An unhealthy diet, smoking, using cocaine or other illegal drugs, heavy alcohol use, and lack of physical activity can raise your risk of heart failure.
- Other medical conditions. Any heart or blood vessel condition, serious lung disease, or infection such as HIV or SARS-CoV-2 may raise your risk of heart failure. Long-term health conditions such as obesity, high blood pressure, diabetes, sleep apnea, chronic kidney disease, anemia, thyroid disease, or iron overload also raise your risk. Cancer treatments such as radiation and chemotherapy can injure your heart and raise your risk. Atrial fibrillation, a common type of irregular heart rhythm, can also cause heart failure.
- Race or ethnicity. African Americans are more likely to have heart failure than people of other races. They also often have more serious cases of heart failure and at a younger age.
- Sex. Heart failure is common in both men and women, although men often develop heart failure at a younger age than women. Women more commonly have heart failure with preserved ejection fraction (HFpEF), which occurs when the heart does not fill with enough blood. Men are more likely to have heart failure with reduced ejection fraction (HFrEF). Women often have worse symptoms than men.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4372
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-16 14:01:00.0
What Is Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle. These diseases have many causes, signs and symptoms, and treatments.
In cardiomyopathy, the heart muscle becomes enlarged, thick, or rigid. In rare cases, the muscle tissue in the heart is replaced with scar tissue.
As cardiomyopathy worsens, the heart becomes weaker. It's less able to pump blood through the body and maintain a normal electrical rhythm. This can lead to heart failure or irregular heartbeats called arrhythmias. In turn, heart failure can cause fluid to build up in the lungs, ankles, feet, legs, or abdomen.
The weakening of the heart also can cause other complications, such as heart valve problems.
Overview
The types of cardiomyopathy are:
- Hypertrophic cardiomyopathy
- Dilated cardiomyopathy
- Restrictive cardiomyopathy
- Arrhythmogenic right ventricular dysplasia
- Unclassified cardiomyopathy
Cardiomyopathy can be acquired or inherited. "Acquired" means you aren't born with the disease, but you develop it due to another disease, condition, or factor. "Inherited" means your parents passed the gene for the disease on to you. Many times, the cause of cardiomyopathy isn't known.
Cardiomyopathy can affect people of all ages. However, people in certain age groups are more likely to have certain types of cardiomyopathy. This article focuses on cardiomyopathy in adults.
Outlook
Some people who have cardiomyopathy have no signs or symptoms and need no treatment. For other people, the disease develops quickly, symptoms are severe, and serious complications occur.
Treatments for cardiomyopathy include lifestyle changes, medicines, surgery, implanted devices to correct arrhythmias, and a nonsurgical procedure. These treatments can control symptoms, reduce complications, and stop the disease from getting worse.
Syndicated Content Details:
Source URL: http://www.nhlbi.nih.gov/subscribe/80216
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-14 20:07:00.0
What are the Signs and Symptoms of Cardiomyopathy?
Some people who have cardiomyopathy never have signs or symptoms. Others don't have signs or symptoms in the early stages of the disease.
As cardiomyopathy worsens and the heart weakens, signs and symptoms of heart failure usually occur. These signs and symptoms include:
- Shortness of breath or trouble breathing, especially with physical exertion
- Fatigue (tiredness)
- Swelling in the ankles, feet, legs, abdomen, and veins in the neck
Other signs and symptoms may include dizziness; light-headedness; fainting during physical activity; arrhythmias (irregular heartbeats); chest pain, especially after physical exertion or heavy meals; and heart murmurs. (Heart murmurs are extra or unusual sounds heard during a heartbeat.)
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4046
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-15 12:57:00.0
What Causes Cardiomyopathy?
Cardiomyopathy can be acquired or inherited. “Acquired” means you aren’t born with the disease, but you develop it due to another disease, condition, or factor.
“Inherited” means your parents passed the gene for the disease on to you. Researchers continue to look for the genetic links to cardiomyopathy and to explore how these links cause or contribute to the various types of the disease.
Many times, the cause of cardiomyopathy isn’t known. This often is the case when the disease occurs in children.
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy usually is inherited. It’s caused by a mutation or change in some of the genes in heart muscle proteins. Hypertrophic cardiomyopathy also can develop over time because of high blood pressure, aging, or other diseases, such as diabetes or thyroid disease. Sometimes the cause of the disease isn’t known.
Dilated Cardiomyopathy
The cause of dilated cardiomyopathy often isn’t known. About one-third of the people who have dilated cardiomyopathy inherit it from their parents.
Certain diseases, conditions, and substances also can cause the disease, such as:
- Alcohol, especially if you also have a poor diet
- Certain toxins, such as poisons and heavy metals
- Complications during the last months of pregnancy
- Ischemic heart disease, heart attack, high blood pressure, diabetes, thyroid disease, viral hepatitis, and HIV
- Illegal drugs, such as cocaine and amphetamines, and some medicines used to treat cancer
- Infections, especially viral infections that inflame the heart muscle
Restrictive Cardiomyopathy
Certain diseases, conditions, and factors can cause restrictive cardiomyopathy, including:
- Amyloidosis: A disease in which abnormal proteins build up in the body’s organs, including the heart
- Connective tissue disorders
- Hemochromatosis: A disease in which too much iron builds up in the body. The extra iron is toxic to the body and can damage the organs, including the heart.
- Sarcoidosis: A disease that causes inflammation and can affect various organs in the body. Researchers believe that an abnormal immune response may cause sarcoidosis. This abnormal response causes tiny lumps of cells to form in the body’s organs, including the heart.
- Some cancer treatments, such as radiation and chemotherapy
Arrhythmogenic Right Ventricular Dysplasia
Researchers think that arrhythmogenic right ventricular dysplasia is an inherited disease.
Syndicated Content Details:
Source URL: http://www.nhlbi.nih.gov/subscribe/4044
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-14 20:10:00.0
Types of Cardiomyopathy
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy is very common and can affect people of any age. Hypertrophic cardiomyopathy affects men and women equally, and about 1 out of every 500 people has the disease.
Hypertrophic cardiomyopathy happens when the heart muscle enlarges and thickens without an obvious cause. Usually the ventricles, the lower chambers of the heart, and septum (the wall that separates the left and right side of the heart) thicken. The thickened areas create narrowing or blockages in the ventricles, making it harder for the heart to pump blood. Hypertrophic cardiomyopathy also can cause stiffness of the ventricles, changes in the mitral valve, and cellular changes in the heart tissue.
Dilated Cardiomyopathy
Dilated cardiomyopathy develops when the ventricles enlarge and weaken. The condition usually starts in the left ventricle and over time can affect the right ventricle. The weakened chambers of the heart don’t pump effectively, causing the heart muscle to work harder. Over time, the heart loses the ability to pump blood effectively. Dilated cardiomyopathy can lead to heart failure, heart valve disease, irregular heart rate, and blood clots in the heart.
Restrictive Cardiomyopathy
Restrictive cardiomyopathy develops when the ventricles become stiff and rigid but the walls of the heart do not thicken. As a result, the ventricles do not relax and don’t fill with the normal blood volume. As the disease progresses, the ventricles do not pump as well and the heart muscle weakens. Over time, restrictive cardiomyopathy can lead to heart failure and problems with the heart valves.
Arrhythmogenic Right Ventricular Dysplasia
Arrhythmogenic right ventricular dysplasia is a rare type of cardiomyopathy that occurs when the muscle tissue in the right ventricle is replaced with fatty or fibrous tissue. This can lead to disruptions in the heart’s electrical signals and causes arrhythmias. Arrhythmogenic right ventricular dysplasia usually affects teens or young adults and can cause sudden cardiac arrest in young athletes.
Unclassified Cardiomyopathy
Other types of cardiomyopathy are grouped into this category and can include:
- Left ventricular noncompaction happens when the left ventricle has trabeculations, projections of muscle inside the ventricle.
- Takotsubo cardiomyopathy, or broken heart syndrome, happens when extreme stress leads to heart muscle failure. Though rare, this condition is more common in post-menopausal women.
Syndicated Content Details:
Source URL: http://www.nhlbi.nih.gov/subscribe/4042
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-14 20:09:00.0
How Is Cardiomyopathy Diagnosed?
Your doctor will diagnose cardiomyopathy based on your medical and family histories, a physical exam, and the results from tests and procedures.
Specialists Involved
Often, a cardiologist or pediatric cardiologist diagnoses and treats cardiomyopathy. A cardiologist specializes in diagnosing and treating heart diseases. A pediatric cardiologist is a cardiologist who treats children.
Medical and Family Histories
Your doctor will want to learn about your medical history. He or she will want to know what signs and symptoms you have and how long you've had them.
Your doctor also will want to know whether anyone in your family has had cardiomyopathy, heart failure, or sudden cardiac arrest.
Physical Exam
Your doctor will use a stethoscope to listen to your heart and lungs for sounds that may suggest cardiomyopathy. These sounds may even suggest a certain type of the disease.
For example, the loudness, timing, and location of a heart murmur may suggest obstructive hypertrophic cardiomyopathy. A "crackling" sound in the lungs may be a sign of heart failure. (Heart failure often develops in the later stages of cardiomyopathy.)
Physical signs also help your doctor diagnose cardiomyopathy. Swelling of the ankles, feet, legs, abdomen, or veins in your neck suggests fluid buildup, a sign of heart failure.
Your doctor may notice signs and symptoms of cardiomyopathy during a routine exam. For example, he or she may hear a heart murmur, or you may have abnormal test results.
Diagnostic Tests
Your doctor may recommend one or more of the following tests to diagnose cardiomyopathy.
Blood Tests
During a blood test, a small amount of blood is taken from your body. It's often drawn from a vein in your arm using a needle. The procedure usually is quick and easy, although it may cause some short-term discomfort.
Blood tests give your doctor information about your heart and help rule out other conditions.
Chest X Ray
A chest x ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels. This test can show whether your heart is enlarged. A chest x ray also can show whether fluid is building up in your lungs.
EKG (Electrocardiogram)
An EKG is a simple test that records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
This test is used to detect and study many heart problems, such as heart attacks, arrhythmias (irregular heartbeats), and heart failure. EKG results also can suggest other disorders that affect heart function.
A standard EKG only records the heartbeat for a few seconds. It won't detect problems that don't happen during the test.
To diagnose heart problems that come and go, your doctor may have you wear a portable EKG monitor. The two most common types of portable EKGs are Holter and event monitors.
Holter and Event Monitors
Holter and event monitors are small, portable devices. They record your heart's electrical activity while you do your normal daily activities. A Holter monitor records the heart's electrical activity for a full 24- or 48-hour period.
An event monitor records your heart's electrical activity only at certain times while you're wearing it. For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
Echocardiography
Echocardiography (echo) is a test that uses sound waves to create a moving picture of your heart. The picture shows how well your heart is working and its size and shape.
There are several types of echo, including stress echo. This test is done as part of a stress test (see below). Stress echo can show whether you have decreased blood flow to your heart, a sign of coronary heart disease.
Another type of echo is transesophageal (tranz-ih-sof-uh-JEE-ul) echo, or TEE. TEE provides a view of the back of the heart.
For this test, a sound wave wand is put on the end of a special tube. The tube is gently passed down your throat and into your esophagus (the passage leading from your mouth to your stomach). Because this passage is right behind the heart, TEE can create detailed pictures of the heart's structures.
Before TEE, you're given medicine to help you relax, and your throat is sprayed with numbing medicine.
Stress Test
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise (or are given medicine if you're unable to exercise) to make your heart work hard and beat fast while heart tests are done.
These tests may include nuclear heart scanning, echo, and positron emission tomography (PET) scanning of the heart.
Diagnostic Procedures
You may have one or more medical procedures to confirm a diagnosis or to prepare for surgery (if surgery is planned). These procedures may include cardiac catheterization (KATH-e-ter-i-ZA-shun), coronary angiography (an-jee-OG-ra-fee), or myocardial (mi-o-KAR-de-al) biopsy.
Cardiac Catheterization
This procedure checks the pressure and blood flow in your heart's chambers. The procedure also allows your doctor to collect blood samples and look at your heart's arteries using x-ray imaging.
During cardiac catheterization, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. This allows your doctor to study the inside of your arteries for blockages.
Coronary Angiography
This procedure often is done with cardiac catheterization. During the procedure, dye that can be seen on an x ray is injected into your coronary arteries. The dye lets your doctor study blood flow through your heart and blood vessels.
Dye also may be injected into your heart chambers. This allows your doctor to study the pumping function of your heart.
Myocardial Biopsy
For this procedure, your doctor removes a piece of your heart muscle. This can be done during cardiac catheterization. The heart muscle is studied under a microscope to see whether changes in cells have occurred. These changes may suggest cardiomyopathy.
Myocardial biopsy is useful for diagnosing some types of cardiomyopathy.
Genetic Testing
Some types of cardiomyopathy run in families. Thus, your doctor may suggest genetic testing to look for the disease in your parents, brothers and sisters, or other family members.
Genetic testing can show how the disease runs in families. It also can find out the chances of parents passing the genes for the disease on to their children.
Genetic testing also may be useful if your doctor thinks you have cardiomyopathy, but you don't yet have signs or symptoms. If the test shows you have the disease, your doctor can start treatment early, when it may work best.
Syndicated Content Details:
Source URL: https://www.nhlbi.nih.gov/subscribe/4047
Source Agency: National Heart, Lung, and Blood Institute (NHLBI)
Captured Date: 2016-03-15 13:12:00.0