Pericarditis & Pericardial Diseases
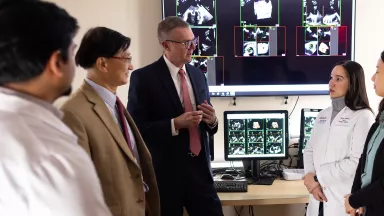
At the Montefiore Einstein Center for Heart and Vascular Care, you can access exceptional care for pericarditis and pericardial diseases. As a global leader in cardiovascular medicine and surgery, we are an academic-based, national and international referral site for high-risk and complex cases. For more than a century, we have been at the forefront in treating heart disease.
Ranked in the top one percent of all hospitals in the nation for Cardiology, Heart & Vascular Surgery according to U.S. News & World Report, our specialists are passionate about uncovering the latest diagnostic approaches and treatments that can improve outcomes. Backed by a multidisciplinary team of specialists, Montefiore Einstein continues to make advances in the treatment of heart disease. In recent years, we have expanded our programs in advanced cardiac imaging, heart failure and interventional cardiovascular medicine and assembled a world-renowned cardiothoracic surgical team.
When you trust us with your care, you can expect compassionate, personalized treatment plans that meet the highest standards for quality and safety. In addition, we offer patients a full choice of support services, from nutritional guidance to rehabilitative therapies.
When you need care for pericarditis and pericardial diseases, turn to our dedicated providers who will develop a highly personalized treatment plan specific to you.
Montefiore Einstein offers the following content from Healthwise’s health information library.
What is pericarditis?
Pericarditis is swelling and irritation of the pericardium, which is the sac that surrounds your heart.
Pericarditis usually doesn't cause serious problems. Most people feel better in a couple of weeks. When there are problems, they may include:
- A buildup of fluid in the pericardial sac. This is called pericardial effusion.
- Sudden pressure on the heart and sudden difficulty pumping enough blood. This is called cardiac tamponade. It can be caused by the weight and pressure of the fluid buildup if it happens quickly.
- Constrictive pericarditis. This happens when the sac around the heart gets thick and stiff. This makes it harder for the heart to pump blood.
What causes it?
Many things can cause pericarditis, including:
- Viral infection. This is the most common cause.
- Heart attack.
- Chest injury.
- Recent heart surgery.
- Certain diseases, such as cancer, lupus, or tuberculosis.
In many cases, the cause is not known.
What are the symptoms?
The main symptom is a sharp pain in the center or left side of your chest. The pain may spread to the shoulder blade. For some people, this pain is dull instead of sharp. It may be worse when you lie down or take a deep breath. The pain usually gets better if you lean forward or sit up.
Other symptoms may include a mild fever, weakness, and feeling very tired.
Pericarditis usually isn't dangerous. But your chest pain could be caused by something more serious, like a heart attack. Getting diagnosed and treated early can help keep pericarditis from leading to other problems. That's why you should call a doctor right away if you have any kind of sudden chest pain.
How is it diagnosed?
Your doctor will listen to your heart during a physical exam. The doctor will also ask questions about your medical history, such as whether you've had a recent illness, radiation treatment for cancer, or tuberculosis. Your doctor may want you to have some tests, including an echocardiogram, electrocardiogram, chest X-ray, and blood tests.
How is pericarditis treated?
If there are no other problems, pericarditis usually goes away on its own in a couple of weeks. During this time:
- Your doctor may prescribe a medicine to relieve pain and reduce inflammation. Medicines may include a nonsteroidal anti-inflammatory drug (NSAID), such as aspirin or ibuprofen, or another type of medicine called colchicine. Be safe with medicines. Read and follow all instructions on the label.
- Get plenty of rest. Avoid exercise and strenuous activity. Ask your doctor when you can be active again.
- Follow your doctor's advice about what problems to watch for, such as shortness of breath or other signs of complications.
Be sure to keep all follow-up appointments with your doctor. If you have complications or the illness gets worse, you may need further treatment. This could include medicines or a procedure to relieve the fluid and pressure around your heart (pericardiocentesis).
Related Videos
Current as of: June 24, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.