Our Approach to Healthy Aging & Degenerative Dementias

The Montefiore Einstein Center for the Aging Brain is internationally recognized for paradigm-shifting research studies that continue to reveal the importance across the lifespan of building and sustaining cognitive resilience through brain and body metabolic regulation; low-level inflammation; novel environmental influences; motor control; cellular and neural network plasticity, and homeostasis and rejuvenation; novel forms of gene and genome regulation; mechanisms of multigenerational inheritance; and exceptionally early developmental influences, including processes mediating the fundamental patterning of a three-dimensional brain and cardinal body axes.
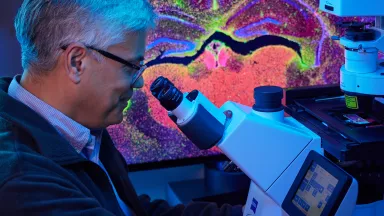
Employing the latest cutting-edge, nano- to whole-brain and body, molecular to structural and functional imaging technologies, our Center for the Aging Brain capitalizes on our institutional commitment to training and nurturing an interdisciplinary team of renowned physician-scientists who integrate rapidly emerging insights regarding brain and body aging, healthspan, sleep-wake biology and circadian rhythms, as well as principles underpinning intellectual resilience and longevity, into a program of comprehensive and evolving interdisciplinary care and dynamic therapeutic optimization.
We are ranked in the top 1% of all hospitals in the nation for neurology and neurosurgery, according to U.S. News & World Report, and our scientific depth and discoveries, breadth of educational programs, and leading clinical care innovations have resulted in recognition as an international referral site for managing complex cases in older adults.
Center of Excellence for Alzheimer’s Disease (CEAD)
At the forefront of research and care of individuals with Alzheimer’s disease or other dementias, the CEAD is one of ten Alzheimer’s Disease Centers of Excellence supported in part by a grant from the New York State Department of Health in an ambitious program to expand knowledge about Alzheimer’s disease and related dementias and improve access to screening, diagnosis and clinical trial opportunities for patients.
The CEAD serves patients from any part of the state or country, but it has a special commitment to the seven counties of the Hudson Valley region including Westchester, Rockland, Putnam, Dutchess, Sullivan, Orange and Ulster counties.

Advanced Treatments
The richness of our culture of scientific innovations, cross-disciplinary scholarship and novel clinical care models has allowed us to continue to advance effective therapeutic interventions where others have failed.
Neurological Services
The Montefiore Einstein Center for the Aging Brain distinguishes itself by fielding a broad-based team of world-renowned experts in the disciplines that impact our understanding of normal aging, healthspan, mechanisms of longevity and the pathophysiology of degenerative dementias. Our academic neurologists have subspecialty expertise in aging and dementia, cognitive neuroscience, neuromuscular medicine, motor control, movement disorders, sleep-wake disorders, headache medicine, neuroimmunology, neurogenetics, metabolic disorders, neuro-ophthalmology, epilepsy and neurovascular disorders.
Our neurologic subspecialists draw upon the expertise of neuroradiology, neurorehabilitation medicine, cardiology, psychiatry and behavioral sciences, geriatrics, bioengineering, systems biology/AI, stem cell biology, epigenetics and regenerative medicine.

Your Center for the Aging Brain Team
The Montefiore Einstein Center for the Aging Brain comprises an elite team of neurologists, neuropsychologists, stroke neurologists, psychiatrists, behavioral therapists, rehabilitation medicine and pain management specialists, board-certified geriatricians, social workers, and nurse consultants, giving patients extensive access to resources for diagnosing, treating and navigating cognitive and other conditions associated with aging.
About Dementia & Alzheimer’s Disease
Dementia is the loss of cognitive functioning—the ability to think, remember or reason—to such an extent that it interferes with a person's daily life and activities. These functions include memory, language skills, visual perception, problem-solving, self-management and the ability to focus and pay attention. Some people with dementia cannot control their emotions, and their personalities may change. Several diseases and conditions can cause dementia or dementia-like symptoms, but dementia itself is not a specific disease.
Alzheimer’s disease is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. In most people with the disease, symptoms first appear when they are in their mid-60s. Early-onset Alzheimer’s occurs between a person’s 30s and mid-60s and is very rare. Alzheimer’s disease is the most common cause of dementia among older adults.