Our Approach to Obstetrical Ultrasound & Fetal Medicine




Montefiore Einstein Obstetrical Ultrasound and Fetal Medicine is a global leader, providing comprehensive, state-of-the-art care for the full range of fetal conditions—from common concerns to the most complex anomalies—including abdominal wall defects, twin-to-twin transfusion syndrome (TTTS), congenital diaphragmatic hernia, fetal growth restriction and complex abnormalities of the brain, lungs and heart. Our multidisciplinary team includes world-renowned physicians who are double board certified in obstetrics and gynecology and maternal-fetal medicine, specializing in the prenatal diagnosis and management of fetal conditions. Our team provides care that is designed to optimize fetal health and support maternal well-being throughout both routine and high-risk pregnancies. We work closely with specialists in neonatology, pediatric cardiology, pediatric surgery, obstetric anesthesiology, obstetric critical care, reproductive and medical genetics and other specialties to deliver seamless, coordinated, patient- and family-centered care.
We are an international referral center for the most complex and high-risk pregnancies—including those involving placenta accreta spectrum (PAS)—and are recognized among the highest performing hospitals in the nation for maternity care, according to U.S. News & World Report. We are a designated Regional Perinatal Center (RPC) and Level 4 Neonatal Intensive Care Unit (NICU) from the New York State Department of Health —one of only 17 RPCs in New York State and one of just 127 Level 4 NICUs nationwide.
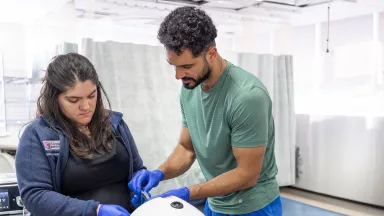
Montefiore Einstein is one of the few hospitals nationwide offering advanced in utero fetal surgeries for high-risk, rare and life-threatening conditions before birth to improve neonatal outcomes. Utilizing the most advanced diagnostic technologies and fetal therapies available, we develop individualized care plans to ensure the best possible outcomes for both mother and baby. Our expertise includes fetoscopic laser surgery for TTTS, radiofrequency ablation (RFA) for twin reversed arterial perfusion (TRAP) sequence, ex utero intrapartum treatment (EXIT) procedures, selective reductions, intrauterine transfusions and shunt placement for bladder or chest drainage. From prenatal diagnosis through delivery and beyond, we are committed to ensuring the safest possible pregnancies and deliveries, providing the highest quality care, optimizing outcomes and promoting the long-term health and well-being of every mother and child.
At the Forefront of Advanced Fetal Diagnostics
We offer comprehensive, same-day fetal diagnostic services—including first-trimester fetal anatomy scans, fetal echocardiography, neurosonography and a full range of prenatal genetic testing. Using state-of-the-art imaging technologies—including high-resolution 3D and 4D ultrasound and Doppler flow studies—our team provides detailed, real-time assessments of fetal anatomy, development, cardiovascular and neurologic function and overall well-being to guide personalized care planning, delivery strategies and timely interventions. Our commitment to excellence in advanced fetal diagnostics enables early detection, supports informed decision-making and promotes the best possible outcomes for both mother and baby.
We are also accredited by the American Institute of Ultrasound in Medicine (AIUM), demonstrating that we exceed nationally recognized standards for the performance and interpretation of diagnostic obstetric and gynecologic ultrasound examinations—and underscoring our commitment to clinical excellence and the highest quality of care. In addition, all of our diagnostic medical sonographers are certified by the American Registry for Diagnostic Medical Sonography (ARDMS), ensuring the highest standards in diagnostic imaging and patient care.
Advancing Care Through Early Detection
Early diagnosis gives families the time to explore their options, meet with our fetal medicine specialists and thoughtfully prepare for complex interventions or specialized deliveries, if needed. Advances in fetal imaging and genetic testing—including chromosomal microarray analysis and next-generation sequencing—allow for the earlier identification of hundreds of genetic syndromes, structural fetal conditions, functional abnormalities and placental disorders such as PAS, placenta previa and other abnormalities of placentation or implantation—empowering families with critical information and a fuller range of choices for care and decision-making.
Clinical Excellence
As a premier academic health system with a specialized Accreta Center, our New York State Department of Health designations as a RPC and Level 4 NICU reflect our commitment to delivering the highest level of maternal and neonatal care for newborns and women with the most complex and high-risk conditions. These distinctions are a testament to our leadership in advanced fetal medicine, high-risk pregnancy management and the exceptional expertise, care and support we provide to all women.

Advanced Diagnostics & Treatments
We offer access to the latest diagnostic technologies, advanced monitoring and innovative treatments to deliver the highest-quality prenatal care for mother and baby.
Our expert team provides comprehensive fetal monitoring and diagnostic evaluations—including biophysical profiles, nonstress tests and Doppler ultrasound studies—to assess fetal well-being, identify potential fetal health risks and guide the development of individualized care plans. We utilize state-of-the-art imaging technologies such as 3D and 4D obstetrical ultrasound, targeted fetal echocardiography, fetal neurosonography and fetal magnetic resonance imaging (MRI), for detailed evaluation of brain, cardiac, thoracic and abdominal anomalies, as well as uterine artery Doppler assessments for early detection of preeclampsia risk.
Our advanced noninvasive prenatal genetic diagnostics include carrier screening before and during pregnancy, first-trimester risk assessment and combined screening, second-trimester quadruple and penta screening and cell-free deoxyribonucleic acid (cfDNA) analysis—commonly referred to as noninvasive prenatal testing (NIPT)—primarily used to screen for common fetal abnormalities such as trisomy 21 (Down syndrome), trisomy 18 and trisomy 13, utilizing next-generation sequencing (NGS) technology. We also specialize in minimally invasive prenatal diagnostic procedures, including chorionic villus sampling, amniocentesis and cordocentesis, supported by chromosomal microarray analysis and, when indicated, diagnostic NGS.
Our specialists support pregnancies requiring advanced medical intervention. This includes coordinated management for PAS, severe preeclampsia or fetal anomalies requiring EXIT procedures. When needed, patients have access to advanced maternal support technologies at our birthing sites—including extracorporeal membrane oxygenation (ECMO) and complex cardiac monitoring—in order to ensure seamless, multidisciplinary care for both mother and baby.
Our team provides specialized care for the full range of fetal conditions, offering advanced diagnostics and therapies, including:
- Comprehensive maternal-fetal evaluation
- Complete medical, obstetric and family history review
- Advanced laboratory testing
- Hormonal and endocrine evaluation
- Coagulation profiles
- Advanced fetal imaging
- High resolution 3D and 4D ultrasound (e.g. for detailed fetal anatomy, evaluation of uterine anomalies, fibroids and early pregnancy complications)
- Doppler flow studies (e.g. to assess placental and fetal circulation)
- Fetal echocardiography (e.g. for detailed assessment of fetal heart structure and function)
- Fetal magnetic resonance imaging—MRI (e.g. for evaluation of complex brain, thoracic or abdominal anomalies)
- Genetic testing
- Carrier screening (before and during pregnancy)
- First-trimester risk assessment/early risk assessment
- Nuchal translucency measurement
- Serum markers (free β-hCG and PAPP-A)
- Second-trimester screening
- Quadruple and penta screening
- Cell-free DNA analysis (cfDNA)/noninvasive prenatal testing (NIPT)
- Next-generation sequencing
- Chromosomal microarray analysis
- Minimally invasive prenatal diagnosis
- Chorionic villus sampling (CVS)
- Amniocentesis
- Cordocentesis (percutaneous umbilical blood sampling)
- Minimally invasive (percutaneous or fetoscopic)
- Minimally invasive fetoscopic laser ablation (e.g. for twin-to-twin transfusion syndrome—TTTS)
- Radiofrequency ablation—RFA (e.g. for twin reversed arterial perfusion—TRAP sequence)
- Selective fetal reductions (e.g. in complicated multiple gestations)
- Fetal blood transfusions (e.g. for severe fetal anemia or hydrops)
- Amnioreduction (e.g. for symptomatic polyhydramnios or TTTS)
- Amnioinfusion (e.g. in cases of oligohydramnios or to improve visualization during procedures)
- In utero shunt placements, including:
- Vesico-amniotic shunts for urinary tract obstruction
- Thoracoamniotic shunts for pleural effusions or congenital pulmonary airway malformation (CPAM)
- Open or ex utero intrapartum treatment (EXIT) surgery
- EXIT procedures (e.g. for fetal airway obstruction)
- Open fetal surgery (e.g. fetal repair of myelomeningocele—spina bifida)
- Advanced fetal therapies
- Fetal balloon tracheal occlusion (e.g. for severe congenital diaphragmatic hernia—CDH)

Research
We are leading collaborative research initiatives and spearheading numerous studies and clinical trials, including several funded by the National Institutes of Health (NIH). Through our clinical trials, patients have access to emerging technologies and innovative treatments that may otherwise be unavailable to the general public.
Our researchers lead basic, translational and clinical investigations to advance fetal medicine and improve outcomes for both mother and baby. Key areas of focus include fetal genetics and developmental biology, prenatal genetic screening and diagnosis, early detection of structural anomalies through advanced ultrasound imaging, fetal therapies for high-risk pregnancies and the integration of genomic medicine into prenatal care. We are also developing and evaluating new diagnostic and therapeutic strategies, including noninvasive fetal monitoring technologies and novel interventions to prevent preterm birth.
In collaboration with our Department of Genetics, our basic science programs are advancing cellular and molecular research—from uncovering mechanisms that contribute to birth defects in 22q11.2 deletion syndrome (22q11.2DS) to leading the nation’s largest pilot newborn screening study of its kind.
Our team has led numerous studies in fetal medicine and prenatal diagnostics. As global principal investigators of the SNP-based Microdeletion and Aneuploidy RegisTry (SMART) Study—the largest multicenter prospective noninvasive prenatal testing (NIPT) study ever conducted and the first large-scale study to collect genetic outcomes in most participants—we investigated the performance of cfDNA screening for the prenatal detection of 22q11.2DS and how high-risk screening results for 22q11.2DS influenced obstetric and neonatal management. We also assessed obstetrical, perinatal and genetic outcomes associated with nonreportable cfDNA screening results.
Additional work includes evaluating the clinical utility of expanded NIPT, the impact of the routine implementation of cfDNA aneuploidy screening on the performance of first-trimester ultrasound and the development of an AI model for early prediction of preeclampsia using cfDNA biomarkers and patient data. In placenta accreta spectrum (PAS) research, we investigated first-trimester screening and used machine learning for the prediction of PAS-related surgical morbidity. We also studied the association between second-trimester fetal abdominal circumference and the prediction of small for gestational age at birth, and examined the association of third-trimester resolution of low placentation and other prenatal ultrasound markers and postpartum hemorrhage with delivery.

Care Navigation & Support Services
Whether you are planning for pregnancy, navigating a high-risk pregnancy or seeking advanced fetal care, our world-renowned team at Montefiore Einstein Fetal Medicine and Ultrasound is here to provide exceptional support, care and resources tailored to your needs.
Our full-service Center offers a comprehensive range of traditional and holistic care before, during and after pregnancy—spanning preconception counseling, screening and prenatal testing through treatment and postpartum recovery. We offer integrated services including social and support programs, genetic counseling and education, care navigation, mental health and wellness support and personalized programs designed to meet each individual’s unique needs.
We are a doula-friendly hospital, offering doula services to support individuals through labor, delivery and postpartum care—helping to ensure the best possible birth outcomes and patient experience. Our Department offers the Women, Infants, and Children (WIC) Program to support the health of low-income women, infants and children up to age 5 who are at nutritional risk by providing free nutritious foods, breastfeeding support, nutrition education and referrals to healthcare and social services.
We also offer a wide range of community-based maternal and child health programs—including Bronx Healthy Start, HealthySteps and the Nurse-Family Partnership, among others—to support families with comprehensive care, education and resources from pregnancy through early childhood, delivered through integrated services that extend beyond the exam room.
Our breadth of resources enables us to deliver highly specialized, coordinated care for both mother and baby—advancing fetal health, supporting maternal well-being, optimizing outcomes and ensuring a healthy pregnancy and the safest delivery possible. Our compassionate and deeply knowledgeable team of physicians, nurses, specialists and support staff is dedicated to guiding you at every step of your pregnancy and fetal care journey.
Your Obstetrical Ultrasound & Fetal Medicine Team
Our multidisciplinary team includes world-renowned physicians who are double board certified in obstetrics and gynecology and maternal-fetal medicine, with subspecialized expertise in fetal medicine. We provide comprehensive, personalized care focused on the diagnosis and treatment of complex fetal conditions—while collaborating closely to ensure the safest possible pregnancies and deliveries, optimize neonatal outcomes and support the long-term health and well-being of both mother and baby.
Transformative Community Programs & Initiatives
Our Program is recognized for its collaborative approach and comprehensive clinical care, which extends beyond the walls of Montefiore Einstein into the community through outreach programs aimed at reducing obstetric risks among vulnerable populations. Specific initiatives include community education on prenatal care and high-risk pregnancy management, collaboration with local hospitals to improve continuity of care for high-risk mothers and participation in policy-making efforts regarding maternal health issues. We continue to expand healthcare access to improve maternal and infant health, preserving continuity of care and reducing disparities for women, children and families.
We work collaboratively with a network of community-based organizations to achieve improved birth outcomes, reduce infant and maternal morbidity and mortality and strengthen healthcare infrastructure in our community. Through the Community Health Worker Institute (CHWI) at Montefiore Einstein, we continue to optimize the integration of community health workers into our clinical care teams to strengthen resources, enhance care coordination and access and improve health outcomes.
One of the unique programs we have spearheaded is called the Bronx Healthy Start Program (BxHSP), a federally-funded program of the Health Resources and Services Administration (HRSA) Maternal & Child Health Bureau that helps pregnant women get the healthcare and support they need during pregnancy and after their baby is born. Mothers and their families are connected to free, voluntary and confidential services including screening and referral for medical services, voluntary home visitation and other resources.
We also offer numerous other community-based maternal and child health programs. HealthySteps supports families by addressing children’s developmental and behavioral needs through integrated, team-based care within the pediatric setting. The Nurse-Family Partnership is a program for low-income, first-time parents, providing home visits and ongoing support from registered nurses during pregnancy until the child turns two years old to improve prenatal, maternal and child health, birth outcomes and early childhood development.
The God’s Love We Deliver Pregnancy and Postpartum Health Program supports high-risk pregnant individuals with gestational or pre-existing diabetes and hypertensive disorders of pregnancy through medical nutrition therapy, nutrition education and counseling and nutritious, medically tailored meals—delivered throughout pregnancy and the postpartum period to promote positive health outcomes for both parent and child.
These are just a few of the many innovative programs we offer to support families during pregnancy and early childhood.
About Fetal Conditions
Fetal conditions encompass a broad range of anomalies and complications that can affect a baby’s development during pregnancy. These may involve the abdominal wall (e.g., gastroschisis, omphalocele), gastrointestinal tract (e.g., bowel or esophageal atresia), genitourinary system (e.g., lower urinary tract obstruction, renal anomalies, polycystic kidney disease), lungs and diaphragm (e.g., congenital diaphragmatic hernia), brain and spine (e.g., congenital brain anomalies, neural tube defects), heart (e.g., fetal arrhythmias, congenital heart defects), and musculoskeletal system (e.g., clubfoot, skeletal dysplasias). Additional concerns include craniofacial anomalies (e.g., cleft lip and cleft palate), hematologic disorders such as fetal anemia, and immune-related conditions like maternal alloimmunization. Some conditions result from chromosomal or genetic abnormalities (e.g., Down syndrome, Edwards syndrome, Patau syndrome, Turner syndrome), while others arise from fetal infections, tumors, fetal growth restriction, or complications of multiple gestations. Advances in prenatal imaging and diagnostics now allow many of these conditions to be identified as early as the first or second trimester. While some congenital anomalies can be effectively managed after birth, others may benefit from close fetal monitoring, in utero treatment, or specialized delivery planning. Early diagnosis enables informed decision-making, coordinated perinatal care, and personalized treatment strategies—which may help to optimize outcomes for infants with complex medical needs.
Fetal Conditions We Treat
Many conditions once considered untreatable can now be diagnosed, managed or even corrected before birth—transforming the outlook for families facing complex fetal diagnoses. While most congenital conditions can be effectively treated after delivery, early prenatal diagnosis, coordinated delivery planning and specialized pre- and postnatal care significantly improve early detection, stabilization and long-term outcomes for infants with complex health needs.
At our Center, we offer comprehensive diagnostic evaluation and multidisciplinary care for a wide range of fetal conditions, including:
- Abdominal wall defects (e.g. gastroschisis, omphalocele)
- Bowel atresia (e.g. duodenal atresia, intestinal atresia)
- Esophageal atresia with or without tracheoesophageal fistula
- Liver or spleen anomalies
- Cardiac tumors
- Congenital heart defects (e.g. hypoplastic left heart syndrome, tetralogy of Fallot)
- Fetal cardiac arrhythmias
- Congenital brain anomalies
- Neural tube defects (e.g. spina bifida (myelomeningocele))
- Abnormal amniotic fluid levels (e.g. oligohydramnios, polyhydramnios)
- Fetal growth restriction
- Cytomegalovirus (CMV)
- Herpes simplex virus (HSV)
- Other (e.g. syphilis, varicella)
- Rubella
- Toxoplasmosis
- Cardiac tumors (e.g. rhabdomyoma)
- Cervical teratoma
- Sacrococcygeal teratoma
- Bladder outlet obstruction (e.g. posterior urethral valves)
- Lower urinary tract obstruction
- Polycystic kidney disease
- Renal anomalies
- Fetal anemia
- Hydrops fetalis
- Maternal immune disorders affecting the fetus
- Monochorionic twins
- Twin reversed arterial perfusion (TRAP)
- Twin-to-twin transfusion syndrome (TTTS)
- Arthrogryposis
- Clubfoot
- Skeletal dysplasias (e.g. osteogenesis imperfecta)
- Placenta accreta spectrum (PAS) disorders
- Placenta previa
- Placental abruption
- Bronchopulmonary sequestration
- Congenital diaphragmatic hernia (CDH)
- Congenital pulmonary airway malformation (CPAM)