Our Approach to Placenta Accreta Spectrum






The Montefiore Einstein Placenta Accreta Spectrum Program is a globally recognized leader, providing comprehensive, individualized care for pregnancies complicated by placenta accreta spectrum (PAS)—one of the most high-risk and complex obstetric conditions. As one of the nation’s most experienced and advanced programs, we specialize in managing a wide range of abnormal placental attachment disorders including placenta accreta, increta and percreta using an individualized approach tailored to the unique needs of each patient. We serve as an international, national and regional referral center for the most complex and challenging PAS cases—offering expert second opinions and streamlined transfer protocols for high-risk pregnancies.
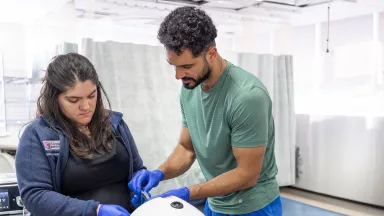
Our dedicated multidisciplinary team includes world-renowned physicians double board certified in obstetrics and gynecology and maternal-fetal medicine. They collaborate closely with neonatologists, gynecologic, pelvic and vascular surgeons, obstetric anesthesiologists, obstetrical critical care specialists, urologists and interventional radiologists to deliver seamless, highly coordinated patient- and family-centered care throughout pregnancy, delivery and postpartum recovery. Recognizing the emotional impact of PAS, we also provide access to prenatal and postpartum fertility preservation counseling and mental health services through our Maternal Behavioral Health Program and Women’s Mental Health Perinatal Intensive Outpatient Program—supporting women and families through diagnosis, treatment and recovery. This 24/7 specialized support ensures the safest and best possible outcomes for both mother and baby.
Montefiore Einstein has earned the Regional Perinatal Center (RPC) and Level 4 Neonatal Intensive Care Unit (NICU) designations from the New York State Department of Health and the American Academy of Pediatrics (AAP). We are one of only 17 RPCs in New York State, one of just 127 Level 4 NICUs nationwide and one of only five Level 4 NICUs in New York City to receive these prestigious recognitions—a reflection of our commitment to delivering the highest level of maternal and neonatal care for women and newborns with the most complex, high-risk conditions. We are among the highest performing hospitals in the nation for maternity care, according to U.S. News & World Report.
Through the integration of advanced prenatal imaging, surgical innovation, evidence-based care protocols and multidisciplinary expertise, we are committed to minimizing maternal and neonatal risks, reducing blood loss, preserving the uterus when clinically appropriate, optimizing outcomes and future fertility and enhancing quality of life for every patient.

Advanced Diagnostics & Treatments
Our comprehensive approach to diagnosis begins with an in-depth maternal-fetal evaluation that includes a detailed review of obstetric, surgical and family medical history, including PAS risk factors, alongside the use of evidence-based risk stratification tools.We offer comprehensive diagnostic services using state-of-the-art imaging technologies—including high-resolution 3D and 4D ultrasound and Doppler flow studies, and magnetic resonance imaging (MRI)—providing detailed, real-time assessments of placental structure, depth of invasion and overall maternal-fetal well-being to guide personalized care planning, delivery strategies and timely interventions. For complex or inconclusive cases, we offer high-resolution pelvic MRI with or without contrast. When bladder or adjacent organ involvement is suspected, targeted diagnostics such as cystoscopy, bladder ultrasound or fetal MRI may be used to guide collaborative surgical planning.
Our advanced laboratory capabilities support diagnosis and risk assessment with comprehensive testing and we also provide fetal echocardiography and other targeted evaluations to ensure detailed prenatal assessment and delivery preparation. We are accredited by the American Institute of Ultrasound in Medicine (AIUM), demonstrating that we exceed nationally recognized standards for the performance and interpretation of diagnostic obstetric and gynecologic ultrasound examinations—and underscoring our commitment to clinical excellence and the highest quality of care.
We offer a full range of the most advanced treatments—ranging from conservative, fertility-sparing options to highly complex surgical interventions—tailored to the specific needs of each patient. For confirmed or high-suspicion PAS cases, we offer scheduled cesarean hysterectomy with the placenta left in situ, particularly in cases of placenta increta or percreta. When clinically appropriate, our team also offers conservative, uterus-sparing options—such as partial myometrial resection, segmental resection with uterine reconstruction or the Triple-P procedure (perioperative placental localization, pelvic devascularization and placental nonseparation). Our surgical team also specializes in minimally invasive, laparoscopic and robot-assisted techniques in select cases. Emerging adjunctive techniques, such as intra-arterial balloon catheter placement and uterine artery embolization, are utilized to reduce intraoperative blood loss and support uterine preservation. Methotrexate therapy may also be considered in select cases of residual placental tissue.
We provide specialized care for the full range of PAS and its associated conditions—offering advanced diagnostics and therapies to support individuals and families from preconception through postpartum recovery. Services include:
- Hysteroscopic resection of the placental remnants
- Intra-arterial balloon catheter placement (internal iliac or uterine artery occlusion by interventional radiology to minimize blood loss)
- Massive hemorrhage protocols
- Antifibrinolytic therapy, fibrinogen concentrates, recombinant activated factor VIIa—rFVIIa (for severe and refractory postpartum hemorrhage)
- Autologous cell-saver technology
- Blood transfusion (packed red blood cells, fresh frozen plasma, platelets)
- Intraoperative cell salvage and autotransfusion including availability of blood products, tranexamic acid (TXA), uterotonics and rapid infusion systems
- Methotrexate therapy
- Uterine artery embolization (may be used intraoperatively or postoperatively to control hemorrhage)
- Uterine artery ligation
- Advanced Imaging
- Cervical length assessment and uterine wall evaluation
- Color and spectral Doppler flow studies (to assess placental and uterine blood flow)
- Fetal echocardiography (if coexisting anomalies or fetal growth restriction is present)
- High-resolution 3D and 4D ultrasound (transabdominal and transvaginal)
- High-resolution pelvic MRI (to assess depth of placental invasion and involvement of adjacent organs)
- Placental mapping and myometrial interface assessment
- Comprehensive maternal-fetal evaluation
- Advanced laboratory testing
- Autoimmune and thrombophilia panel when clinically indicated
- Coagulation profiles and platelet function testing
- Coagulation tests
- Platelet function assays
- Viscoelastic testing using thromboelastography or rotational thromboelastometry
- Diabetes screening
- Hormonal and endocrine evaluation
- Infectious disease screening (e.g. human immunodeficiency virus—HIV, hepatitis B/C, syphilis, rubella)
- Maternal serum markers
- Alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), PAPP-A
- Urine and vaginal screening (e.g. urinalysis, sexually transmitted infection—STI panel, group B streptococcus—GBS culture)
- Detailed medical, obstetric and family history review
- Integration of obstetric history and key risk factors (e.g. prior cesarean deliveries, placenta previa, uterine surgery, assisted reproductive technologies including in vitro fertilization—IVF)
- Risk stratification tools
- Standardized scoring systems combining imaging and clinical risk factors
- Advanced laboratory testing
- Cystoscopy (performed in select cases of suspected bladder invasion—placenta percreta)
Advanced Treatments
- Family support services, including counseling for partners and caregivers
- Maternal Behavioral Health Program for individualized mental health support before and after delivery
- Postpartum recovery planning, including structured follow-up and emotional wellness resources
- Reproductive and fertility counseling post-hysterectomy or conservative surgery
- Women’s Mental Health Perinatal Intensive Outpatient Program
- Bladder or bowel repair or resection (in cases of placenta percreta involving adjacent organs)
- Delayed interval cesarean hysterectomy
- Minimally invasive techniques (laparoscopic and robot-assisted)
- Modified radical or total hysterectomy
- Planned cesarean hysterectomy (uterus with placenta left in situ and removed en bloc to prevent hemorrhage; often performed between 34 and 36 weeks gestation)
- Conservative management (removal of placenta or uteroplacental tissue without removal of the uterus)
- Minimally invasive techniques (laparoscopic and robot-assisted)
- Partial myometrial resection with uterine reconstruction
- Segmental uterine resection
- The Triple-P procedure (perioperative placental localization, pelvic devascularization and placental nonseparation)
- Expectant management (placenta left in situ—leaving the placenta either partially or totally in situ)
Research & Clinical Trials
We are leading collaborative research initiatives and spearheading numerous studies and clinical trials, including several funded by the National Institutes of Health (NIH). Through our clinical trials, patients have access to emerging technologies and innovative treatments that may otherwise be unavailable to the general public.
Our researchers lead basic, translational and clinical investigations to advance the understanding of PAS and improve outcomes for both mother and baby. Key areas of focus include early detection of placental invasion and structural anomalies through advanced imaging techniques, and the development of innovative therapies and new approaches to managing high-risk pregnancies.
We investigated first-trimester screening and used machine learning for the prediction of PAS-related surgical morbidity. We also studied the association between second-trimester fetal abdominal circumference and the prediction of small for gestational age (SGA) at birth, and examined the association of third-trimester resolution of low placentation and other prenatal ultrasound markers and postpartum hemorrhage with delivery.

Care Navigation & Support Services
Whether you’re at risk for or have been diagnosed with PAS, navigating a high-risk pregnancy or recovering after a PAS-related delivery, our world-renowned team at the Montefiore Einstein Placenta Accreta Spectrum Program is here to provide exceptional support, care and resources tailored to your needs.
Our full-service program offers a comprehensive range of traditional and holistic care before, during and after pregnancy—spanning preconception counseling, screening and prenatal testing through treatment and postpartum recovery. We offer integrated services including social and support programs, genetic counseling and education, care navigation, mental health and wellness support and personalized programs designed to meet each individual’s unique needs.
We are a doula-friendly hospital, offering doula services to support individuals through labor, delivery and postpartum care—helping to ensure the best possible birth outcomes and patient experience. Our Department offers the Women, Infants and Children (WIC) Program to support the health of low-income women, infants and children up to age 5 who are at nutritional risk by providing free nutritious foods, breastfeeding support, nutrition education and referrals to healthcare and social services.
We also offer a wide range of community-based maternal and child health programs—including Bronx Healthy Start, HealthySteps and the Nurse-Family Partnership, among others—to support families with comprehensive care, education and resources from pregnancy through early childhood, delivered through integrated services that extend beyond the exam room.
Our breadth of resources enables us to deliver highly specialized, coordinated care for both mother and baby—advancing fetal health, supporting maternal well-being, optimizing outcomes and ensuring a healthy pregnancy and the safest delivery possible. Our compassionate and deeply knowledgeable team of physicians, nurses, specialists and support staff is dedicated to guiding you at every step of your perinatal care journey.
Your Placenta Accreta Spectrum Program Team
Our multidisciplinary team includes world-renowned physicians double board certified in obstetrics and gynecology and maternal-fetal medicine, who collaborate closely with neonatologists, gynecologic, pelvic and vascular surgeons, obstetric anesthesiologists, obstetrical critical care specialists, urologists, interventional radiologists and other experts with specialized expertise in diagnosing and managing PAS and its associated complications to help ensure the safest and best possible outcomes for both mother and baby.
About Placenta Accreta Spectrum
Placenta accreta spectrum (PAS) is one of the most complex and challenging obstetric conditions, encompassing various degrees of abnormal adherence and invasion of the placenta into or beyond the muscular wall (myometrium) of the uterus. In PAS, the placenta does not detach spontaneously after delivery and cannot be manually removed without risking massive, potentially life-threatening bleeding. The condition represents a spectrum of disorders and is classified into three main types based on the depth of myometrial invasion: placenta accreta (attachment and adherence to the myometrium without invasion), placenta increta (invasion into the myometrium) and placenta percreta (penetration through the uterine wall, often involving adjacent organs such as the bladder or bowel).
PAS most often occurs in individuals with a history of prior cesarean deliveries and other uterine surgeries—such as myomectomy or dilation and curettage—placenta previa, advanced maternal age, multiparity, Asherman’s syndrome and IVF. Early and accurate diagnosis is critical, as PAS presents significant risks to both maternal and fetal health, including severe hemorrhage during and after delivery, emergency hysterectomy and subsequent loss of future fertility, urinary tract injury and other organ damage, preterm birth and complications requiring intensive care for both mother and baby. The psychological impacts of PAS can also be profound.
Because of these risks, PAS requires early recognition whenever possible, a multifaceted diagnostic approach and highly coordinated multidisciplinary care. Careful prenatal planning and expert management are essential to mitigate maternal and neonatal complications, preserve fertility when clinically appropriate and ensure the safest and best possible outcomes for both mother and baby.