Extracranial Germ Cell Tumors Treatment
If your child has been diagnosed with an extracranial germ cell tumor—a cancerous or noncancerous growth that develops outside of the brain in a type of cell that normally becomes either sperm or egg—you can depend on the expert care provided at Montefiore Einstein Comprehensive Cancer Center at the Children’s Hospital at Montefiore Einstein (CHAM).
Our multidisciplinary and collaborative approach to research and treatment ensures your child will receive the best care. We offer the most advanced treatments available, including clinical trials. We’re actively engaged in defining the next generation of treatment.
With exceptional physicians, nurses, specialists and support staff, our multidisciplinary and collaborative approach to treatment ensures your child will receive the best care in a supportive and nurturing environment.
When you want only the best for your child, turn to the caring specialists at Montefiore Einstein Comprehensive Cancer Center at CHAM, who are passionate about ending cancer and addressing your child’s whole health needs.

Cancer Clinical Trials
- Blood & Bone Marrow Cancers
- Brain, Spine & Central Nervous System Cancers
- Breast Cancer
- Childhood Cancers
- Endocrine System Cancers
- Gastrointestinal (GI) Cancers
- Genitourinary (GU) & Urologic Cancers
- Gynecologic Cancers
- Head & Neck Cancers
- Kaposi Sarcoma & AIDS-Related Cancers
- Lung & Chest Cancers
- Prostate Cancer
- Sarcomas
- Skin Cancer
As an NCI-designated comprehensive cancer center, Montefiore Einstein Comprehensive Cancer Center supports the mission and guidelines of the National Cancer Institute (NCI). The following information about types of cancer, prevention and treatments is provided by the NCI.
Childhood Extracranial Germ Cell Tumors Treatment (PDQ®)–Patient Version
General Information About Childhood Extracranial Germ Cell Tumors
Key Points
- Childhood extracranial germ cell tumors start in germ cells in parts of the body other than the brain.
- Childhood extracranial germ cell tumors may be benign or malignant.
- Childhood extracranial germ cell tumors are grouped as gonadal or extragonadal extracranial tumors.
- Gonadal germ cell tumors
- Extragonadal extracranial germ cell tumors
- There are three types of extracranial germ cell tumors.
- Teratomas
- Malignant germ cell tumors
- Mixed germ cell tumors
- The cause of most childhood extracranial germ cell tumors is unknown.
- Having certain inherited disorders can increase the risk of extracranial germ cell tumors.
- Signs of childhood extracranial germ cell tumors depend on where the tumor formed in the body.
- Imaging studies and blood tests are used to diagnose childhood extracranial germ cell tumors.
- Certain factors affect prognosis (chance of recovery) and treatment options.
Childhood extracranial germ cell tumors start in germ cells in parts of the body other than the brain.
A germ cell is a type of cell that forms as a fetus develops. These cells later become sperm in the testicles or eggs in the ovaries.
This summary is about germ cell tumors that form in parts of the body that are extracranial (outside the brain). Extracranial germ cell tumors usually form in the following areas of the body:
- Testicles.
- Ovaries.
- Sacrum or coccyx (tailbone).
- Retroperitoneum (area in the back of the abdomen behind the tissue that lines the abdominal wall and covers most of the organs in the abdomen).
- Mediastinum (area between the lungs).
- Head and neck.
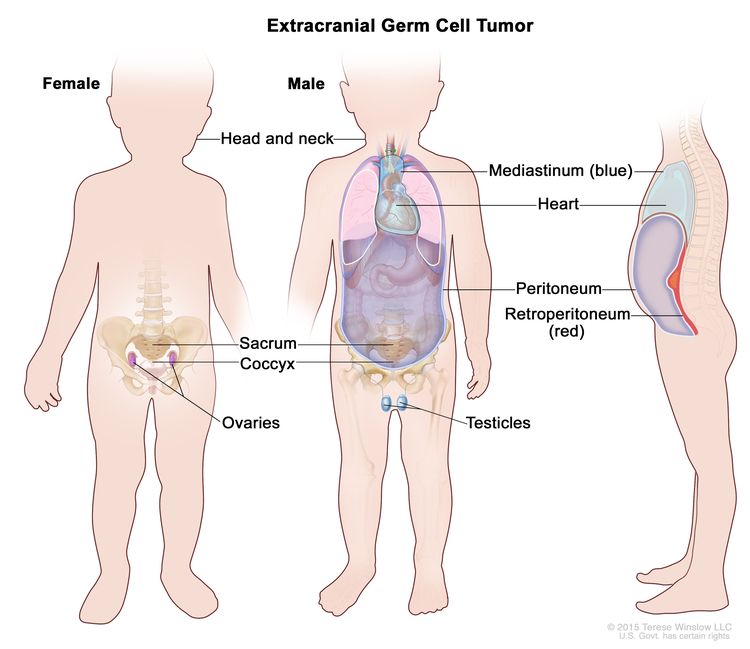
Extracranial germ cell tumors form in parts of the body other than the brain. This includes the testicles, ovaries, sacrum (lower part of the spine), coccyx (tailbone), mediastinum (area between the lungs), retroperitoneum (the back wall of the abdomen), and the head and neck.
Extracranial germ cell tumors are most common in adolescents, with rates in this age group lower for females than males.
For information on intracranial (inside the brain) germ cell tumors, see Childhood Central Nervous System Germ Cell Tumors Treatment.
Childhood extracranial germ cell tumors may be benign or malignant.
Extracranial germ cell tumors may be benign (noncancer) or malignant (cancer).
Childhood extracranial germ cell tumors are grouped as gonadal or extragonadal extracranial tumors.
Malignant extracranial germ cell tumors are tumors that form outside the brain. They are gonadal or extragonadal.
Gonadal germ cell tumors
Gonadal germ cell tumors form in the gonads (testicles and ovaries).
- Testicular germ cell tumors. Testicular germ cell tumors are divided into two main types, seminoma and nonseminoma. Nonseminomas are usually large and cause signs or symptoms of disease. They tend to grow and spread more quickly than seminomas.
Testicular germ cell tumors usually occur before the age of 5 years or in adolescents and young adults. Testicular germ cell tumors in adolescents (11 years and older) and young adults are different from those that form in early childhood.
- Ovarian germ cell tumors. Ovarian germ cell tumors are more common in adolescent girls and young women. Most ovarian germ cell tumors are benign mature teratomas (dermoid cysts). Some ovarian germ cell tumors, such as immature teratomas, dysgerminomas, yolk sac tumors, or mixed germ cell tumors, are malignant.
Extragonadal extracranial germ cell tumors
Extragonadal extracranial germ cell tumors form in areas of the body other than the brain or gonads (testicles and ovaries).
Most extragonadal extracranial germ cell tumors form along the midline of the body. This includes the following:
- Sacrum (the large, triangle-shaped bone in the lower spine that forms part of the pelvis).
- Coccyx (tailbone).
- Mediastinum (the area between the lungs).
- Back of the abdomen.
- Neck.
In children younger than 11 years, extragonadal extracranial germ cell tumors usually occur at birth or in early childhood. Most of these tumors are benign teratomas in the sacrum or coccyx.
In older children, adolescents, and young adults (11 years and older), extragonadal extracranial germ cell tumors are often in the mediastinum.
There are three types of extracranial germ cell tumors.
Extracranial germ cell tumors are also grouped into teratomas, malignant germ cell tumors, and mixed germ cell tumors:
Teratomas
There are two main types of teratomas:
- Mature teratomas. These tumors are the most common type of extracranial germ cell tumor. Mature teratomas are benign tumors and not likely to become cancer. They usually occur in the sacrum or coccyx in newborns or in the testicles or ovaries at the start of puberty. The cells of mature teratomas look almost like normal cells under a microscope. Some mature teratomas release enzymes or hormones that cause signs and symptoms of disease.
- Immature teratomas. These tumors usually occur in areas other than the gonads in young children or in the ovaries at the start of puberty. They have cells that look very different from normal cells under a microscope. Immature teratomas may be cancer and spread to other parts of the body. They often have several different types of tissue in them, such as hair, muscle, and bone. Some immature teratomas release enzymes or hormones that cause signs and symptoms of disease.
Malignant germ cell tumors
Malignant germ cell tumors are cancer. There are two main types of malignant germ cell tumors:
- Seminomatous germ cell tumors. There are three types of seminomatous germ cell tumors:
- Seminomas form in the testicle.
- Dysgerminomas form in the ovary.
- Germinomas form in areas of the body that are not the ovary or testicle, such as the mediastinum.
- Nonseminomatous germ cell tumors. There are four types of nonseminomatous germ cell tumors:
- Yolk sac tumors make a hormone called alpha-fetoprotein (AFP). They can form in the ovary, testicle, or other areas of the body.
- Choriocarcinomas make a hormone called beta-human chorionic gonadotropin (beta-hCG). They can form in the ovary, testicle, or other areas of the body.
- Embryonal carcinomas may make a hormone called beta-hCG. They can form in the testicle or other areas of the body, but not in the ovary.
- Gonadoblastomas can form in the ovary.
Mixed germ cell tumors
Mixed germ cell tumors are made up of at least two types of malignant germ cell tumor. They can form in the ovary, testicle, or other areas of the body.
The cause of most childhood extracranial germ cell tumors is unknown.
Having certain inherited disorders can increase the risk of extracranial germ cell tumors.
A risk factor is anything that increases the chance of getting a disease. Not every child with one or more of these risk factors will develop an extracranial germ cell tumor. And it will develop in some children who don't have a known risk factor.
Possible risk factors for extracranial germ cell tumors include:
- Having certain genetic syndromes:
- Klinefelter syndrome may increase the risk of germ cell tumors in the mediastinum.
- Swyer syndrome may increase the risk of gonadoblastoma and seminoma.
- Turner syndrome may increase the risk of gonadoblastoma and dysgerminoma.
- Having an undescended testicle may increase the risk of testicular cancer.
- Having an ovary or testicle that has not formed normally (gonadal dysgenesis) may increase the risk of gonadoblastoma.
Talk with your child's doctor if you think your child may be at risk.
Signs of childhood extracranial germ cell tumors depend on where the tumor formed in the body.
Different tumors may cause the following signs and symptoms. Other conditions may cause these same signs and symptoms. It's important to check with your child's doctor if your child has:
- A lump in the neck, abdomen, or lower back.
- A painless lump in the testicle.
- Pain in the abdomen or back.
- Respiratory distress, chest pain, or cough.
- Fever.
- Constipation.
- Trouble urinating.
- Early puberty.
- In females, no menstrual periods or unusual vaginal bleeding.
Imaging studies and blood tests are used to diagnose childhood extracranial germ cell tumors.
If your child has symptoms that suggest they have an extracranial germ cell tumor, their doctor will need to find out if these are due to cancer or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will also ask about your child's personal and family medical history and do a physical exam. Depending on these results, they may recommend other tests. If your child is diagnosed with an extracranial germ cell tumor, the results of these tests will help you and your child's doctor plan treatment.
The tests used to diagnose extracranial germ cell tumors may include:
- Serum tumor marker test: A procedure in which a sample of blood is checked to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers.
Some malignant germ cell tumors release tumor markers. The following tumor markers may be used to detect extracranial germ cell tumors:
- Alpha-fetoprotein (AFP).
- Beta-human chorionic gonadotropin (beta-hCG).
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body, including lactate dehydrogenase. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the chest or lymph nodes, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
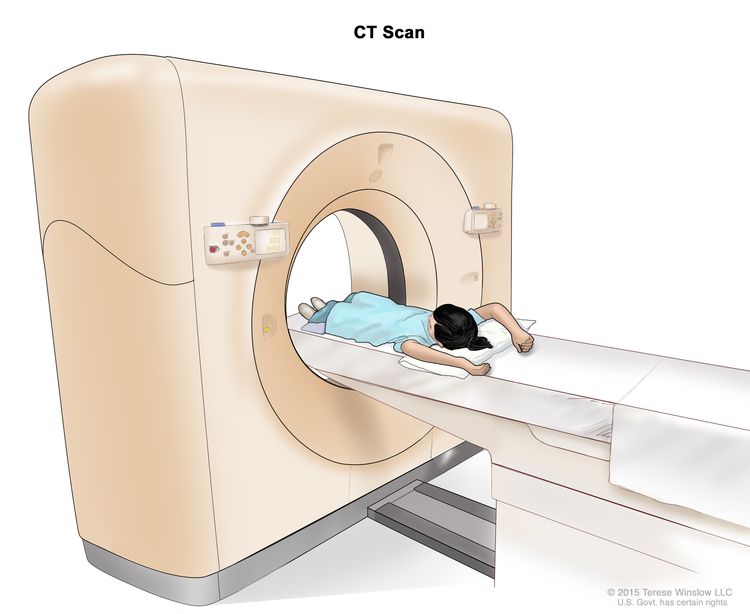
Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
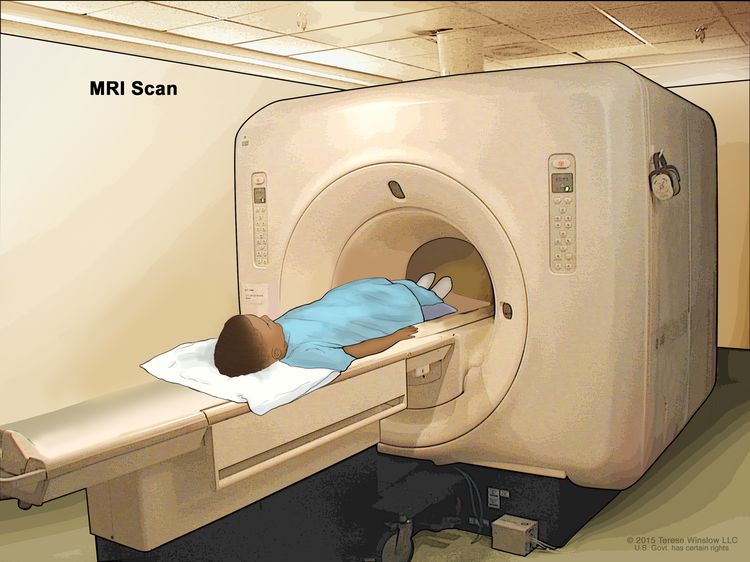
Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
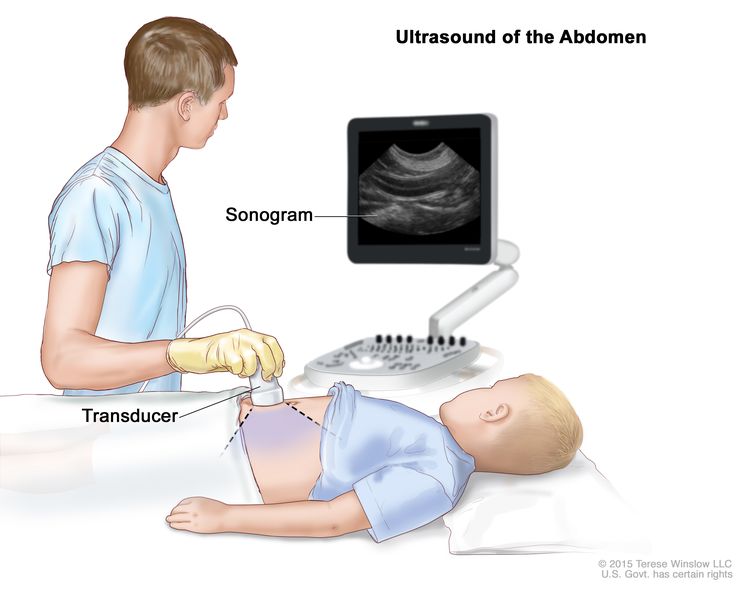
Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture).
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. Sometimes an incisional biopsy or needle biopsy is done before surgery to remove a sample of tissue. Sometimes the tumor is removed during surgery and then a sample of tissue is removed from the tumor.
The following tests may be done on the sample of tissue that is removed:
- Cytogenetic analysis: A laboratory test in which the chromosomes of cells in a sample of tissue are counted and checked for any changes, such as broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of cancer. Cytogenetic analysis is used to help diagnose cancer, plan treatment, or find out how well treatment is working.
- Immunohistochemistry: A laboratory test that uses antibodies to check for certain antigens (markers) in a sample of a patient's tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on the following:
- The child's age and general health.
- The stage of the cancer (whether it has spread to nearby areas, lymph nodes, or to other places in the body).
- Where the tumor first began to grow.
- The type of germ cell tumor.
- How well the tumor responds to treatment.
- Whether the child has gonadal dysgenesis.
- Whether the tumor can be completely removed by surgery.
- Whether the cancer has just been diagnosed or has recurred (come back).
The prognosis for childhood extracranial germ cell tumors, especially ovarian germ cell tumors, is good.
Stages of Childhood Extracranial Germ Cell Tumors
Key Points
- After a childhood extracranial germ cell tumor has been diagnosed, tests are done to find out if cancer cells have spread from where the tumor started to nearby areas or to other parts of the body.
- There are three ways that cancer spreads in the body.
- Cancer may spread from where it began to other parts of the body.
- Stages are used to describe the different types of extracranial germ cell tumors.
- Testicular germ cell tumors in children younger than 11 years
- Testicular germ cell tumors in adolescents and young adults 11 years and older
- Ovarian germ cell tumors
- Extragonadal extracranial germ cell tumors
- Childhood extracranial germ cell tumors usually do not come back after treatment.
After a childhood extracranial germ cell tumor has been diagnosed, tests are done to find out if cancer cells have spread from where the tumor started to nearby areas or to other parts of the body.
The process used to find out if cancer has spread from where the tumor started to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment. In some cases, staging may follow surgery to remove the tumor.
The following procedures may be used:
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the brain or lymph nodes. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the chest or lymph nodes, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Bone scan: A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
- Thoracentesis: The removal of fluid from the space between the lining of the chest and the lung, using a needle. A pathologist views the fluid under a microscope to look for cancer cells.
- Paracentesis: The removal of fluid from the space between the lining of the abdomen and the organs in the abdomen, using a needle. A pathologist views the fluid under a microscope to look for cancer cells.
The results from tests and procedures used to detect and diagnose childhood extracranial germ cell tumors may also be used in staging.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if an extracranial germ cell tumor spreads to the liver, the cancer cells in the liver are actually cancerous germ cells. The disease is metastatic extracranial germ cell tumor, not liver cancer.
Stages are used to describe the different types of extracranial germ cell tumors.
Testicular germ cell tumors in children younger than 11 years
The following stages are from the Children's Oncology Group.
- Stage I
In stage I, the cancer is found in the testicle only. The testicle and spermatic cord are completely removed by surgery and all of the following are true:
- the capsule (outer covering of the tumor) did not rupture (break open) and a biopsy was not done before the tumor was removed; and
- all lymph nodes are smaller than 1 centimeter in their shortest diameter on a CT scan or MRI.
- Stage II
In stage II, the testicle and spermatic cord are removed by surgery and one of the following is true:
- the capsule (outer covering of the tumor) ruptured (broke open) or a biopsy was done before surgery; or
- cancer that can only be seen with a microscope remains in the scrotum or in the spermatic cord near the scrotum, and after surgery, tumor marker levels do not return to normal or do not decrease.
Cancer has not spread to the lymph nodes.
- Stage III
In stage III, one of the following is true:
- the cancer has spread to one or more lymph nodes at the back of the abdomen; or
- lymph nodes are at least 2 centimeters wide or are larger than 1 centimeter but smaller than 2 centimeters in their shortest diameter and either have not changed or are growing when a CT scan or MRI is repeated within 4 to 6 weeks.
- Stage IV
In stage IV, the cancer has spread to other parts of the body, such as the liver, lung, bone, and brain.
Testicular germ cell tumors in adolescents and young adults 11 years and older
In males older than 15 years, there are only stage I tumors and metastatic tumors. For more information about staging used for testicular germ cell tumors in adolescents and young adults 11 years and older, see Testicular Cancer Treatment.
Ovarian germ cell tumors
Two staging systems are used for ovarian germ cell tumors: Children's Oncology Group and the International Federation of Gynecology and Obstetrics (FIGO).
The following stages are from the Children's Oncology Group.
- Stage I
In stage I, the tumor in the ovary is completely removed by surgery and all of the following are true:
- the capsule (outer covering of the tumor) did not rupture (break open) and a biopsy was not done before the tumor was removed; and
- there is no sign that the cancer has spread through the capsule; and
- no cancer cells are found in fluid taken from the abdomen; and
- no cancer is seen in tissue that lines the abdomen or found in tissue samples taken during a biopsy; and
- lymph nodes are smaller than 1 centimeter in their shortest diameter on a CT scan or MRI or no cancer is found in lymph node tissue samples taken during a biopsy.
- Stage II
In stage II, the tumor in the ovary is completely removed by surgery and a biopsy is done before surgery and one of the following is true:
- cancer has spread through part or all of the capsule (outer covering of the tumor); or
- the tumor is larger than 10 centimeters and is removed by laparoscopic surgery; or
- the tumor is removed by being broken up into small pieces and it is not known if cancer has spread through the capsule.
Cancer cells are not found in fluid taken from the abdomen. Cancer is not seen in lymph nodes or tissue that lines the abdomen and cancer is not found in tissue samples taken during a biopsy.
- Stage III
In stage III, there is tumor in the ovary and one of the following is true:
- lymph nodes are at least 2 centimeters wide or are larger than 1 centimeter but smaller than 2 centimeters in their shortest diameter and either have not changed or are growing when a CT scan or MRI is repeated 4 to 6 weeks after surgery; or
- the tumor is not completely removed by surgery or a biopsy was done before surgery; or
- cancer cells (including immature teratoma) are found in fluid taken from the abdomen; or
- cancer (including immature teratoma) is found in lymph nodes; or
- cancer (including immature teratoma) is found in tissue that lines the abdomen.
- Stage III-X
In stage III-X, the tumor can be described as stage I or stage II, except:
- cells lining the abdomen were not collected; or
- a biopsy of lymph nodes larger than 1 centimeter in their shortest diameter was not done; or
- a biopsy of tissue from the lining of the abdomen was not done; or
- staging was not completed during surgery but will be completed during a second surgery.
- Stage IV
In stage IV, one of the following is true:
The following stages are from the International Federation of Gynecology and Obstetrics (FIGO).
- Stage I
In stage I, cancer is found in one or both of the ovaries and has not spread. Stage I is divided into stage IA, stage IB, and stage IC.
- Stage IA: Cancer is found in one ovary.
- Stage IB: Cancer is found in both ovaries.
- Stage IC: Cancer is found in one or both ovaries and one of the following is true:
- cancer is also found on the outside surface of one or both ovaries; or
- the capsule (outer covering) of the tumor ruptured (broke open) before or during surgery; or
- cancer cells are found in fluid taken from the abdomen or in washings of the peritoneal cavity (the body cavity that contains most of the organs in the abdomen).
- Stage II
In stage II, cancer is found in one or both ovaries and has spread into other areas of the pelvis, or primary peritoneal cancer is found. Stage II is divided into stage IIA and stage IIB.
- Stage III
In stage III, cancer is found in one or both ovaries or primary peritoneal cancer is found. Cancer has spread outside the pelvis to other parts of the abdomen and/or to lymph nodes at the back of the abdomen. Stage III is divided into stage IIIA, stage IIIB, and stage IIIC.
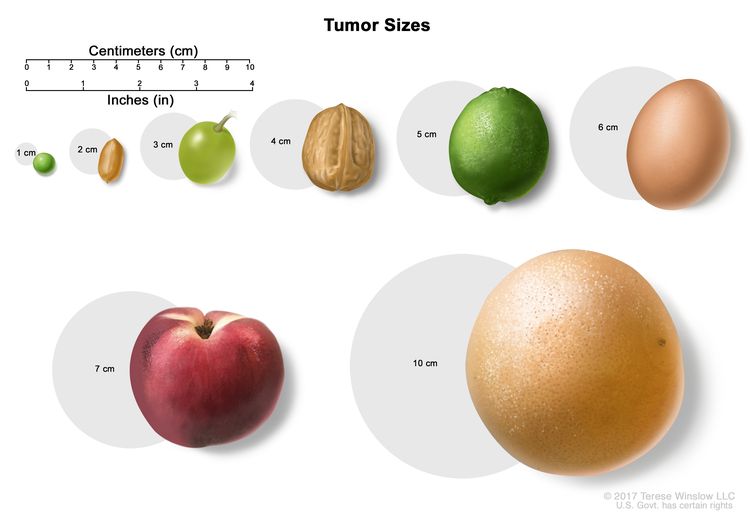
Tumor sizes are often measured in centimeters (cm) or inches. Common food items that can be used to show tumor size in cm include: a pea (1 cm), a peanut (2 cm), a grape (3 cm), a walnut (4 cm), a lime (5 cm or 2 inches), an egg (6 cm), a peach (7 cm), and a grapefruit (10 cm or 4 inches).
- In stage IIIA, one of the following is true:
- cancer has spread to lymph nodes at the back of the abdomen only; or
- cancer cells that can be seen only with a microscope have spread to the surface of the peritoneum outside the pelvis. Cancer may have spread to nearby lymph nodes at the back of the abdomen.
- Stage IIIB: Cancer has spread to the peritoneum outside the pelvis and the cancer in the peritoneum is 2 centimeters or smaller. Cancer may have spread to lymph nodes at the back of the abdomen.
- Stage IIIC: Cancer has spread to the peritoneum outside the pelvis and the cancer in the peritoneum is larger than 2 centimeters. Cancer may have spread to lymph nodes at the back of the abdomen or to the surface of the liver or spleen.
- In stage IIIA, one of the following is true:
- Stage IV
Stage IV is divided into stage IVA and IVB.
Extragonadal extracranial germ cell tumors
The following stages are from the Children's Oncology Group.
- Stage I
In stage I, the tumor is completely removed by surgery and all of the following are true:
- no cancer cells are found in the area where the tumor was removed; and
- the capsule (outer covering of the tumor) did not rupture (break open) and a biopsy was not done before the tumor was removed; and
- cancer cells are not found in fluid taken from the abdominal cavity, if the tumor is in the abdomen; and
- lymph nodes are smaller than 1 centimeter on a CT scan or MRI of the abdomen, pelvis, and chest.
- Stage II
In stage II, cancer is not completely removed by surgery and one of the following is true:
- cancer that can only be seen with a microscope remains after surgery; or
- the capsule (outer covering of the tumor) ruptured (broke open) or a biopsy was done.
Cancer cells are not found in fluid taken from the abdomen. There is no sign of cancer in lymph nodes in the abdomen, pelvis, or chest on a CT scan or MRI.
- Stage III
In stage III, one of the following is true:
- cancer is not completely removed by surgery and cancer that can be seen with the eye remains after surgery or only a biopsy was done; or
- lymph nodes are at least 2 centimeters wide or are larger than 1 centimeter but smaller than 2 centimeters in their shortest diameter and either have not changed or are growing when a CT scan or MRI is repeated within 4 to 6 weeks.
- Stage IV
In stage IV, the cancer has spread to other parts of the body, such as the liver, lung, bone, or brain.
Childhood extracranial germ cell tumors usually do not come back after treatment.
Recurrent childhood extracranial germ cell tumor is cancer that has come back after it has been treated. The cancer may come back in the same place or in other parts of the body.
Most germ cell tumors do not recur (come back) after treatment. If they do recur, they usually come back within 3 years of surgery. About half of the teratomas that recur in the sacrum or coccyx are cancer, so follow-up is important.
Treatment Option Overview
Key Points
- There are different types of treatment for children with extracranial germ cell tumors.
- Children with extracranial germ cell tumors should have their treatment planned by a team of health care providers who are experts in treating cancer in children.
- The following types of treatment are used:
- Surgery
- Observation
- Chemotherapy
- New types of treatment are being tested in clinical trials.
- High-dose chemotherapy with stem cell transplant
- Radiation therapy
- Treatment for childhood extracranial germ cell tumors may cause side effects.
- Patients may want to think about taking part in a clinical trial.
- Patients can enter clinical trials before, during, or after starting their cancer treatment.
- Follow-up tests may be needed.
There are different types of treatment for children with extracranial germ cell tumors.
Different types of treatments are available for children with extracranial germ cell tumors. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Children with extracranial germ cell tumors should have their treatment planned by a team of health care providers who are experts in treating cancer in children.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other health care providers who are experts in treating children with extracranial germ cell tumors and who specialize in certain areas of medicine. These may include the following specialists:
The following types of treatment are used:
Surgery
Surgery to completely remove the tumor is done whenever possible. If the tumor is very large, chemotherapy may be given first, to make the tumor smaller and decrease the amount of tissue that needs to be removed during surgery. A goal of surgery is to keep reproductive function. The following types of surgery may be used:
- Resection: Surgery to remove tissue or part or all of an organ.
- Radical inguinal orchiectomy: Surgery to remove one or both testicles through an incision (cut) in the groin.
- Unilateral salpingo-oophorectomy: Surgery to remove one ovary and one fallopian tube on the same side.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy after surgery to kill any cancer cells that are left. Treatment given after surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Observation
Observation is closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change. For children with extracranial germ cell tumors, this includes physical exams, imaging tests, and tumor marker tests.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). Systemic chemotherapy is used to treat extracranial germ cell tumors.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Learn more at Clinical Trials Information for Patients and Caregivers.
High-dose chemotherapy with stem cell transplant
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
Radiation therapy
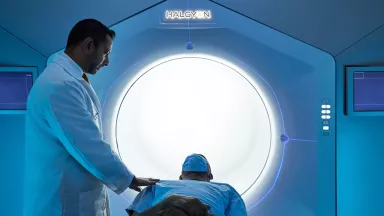
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. External radiation therapy is being studied for the treatment of childhood extracranial germ cell tumors that have come back.
Treatment for childhood extracranial germ cell tumors may cause side effects.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following:
- Physical problems, such as infertility, trouble hearing and kidney problems.
- Changes in mood, feelings, thinking, learning, or memory.
- Second cancers (new types of cancer), such as leukemia or malignant melanoma.
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
As your child goes through treatment, they will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back).
For childhood extracranial germ cell tumors, follow-up may include regular physical exams, tumor marker tests, and imaging tests such as CT scan, MRI or chest x-ray.
Treatment of Childhood Mature and Immature Teratomas
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed mature teratomas includes the following:
- Surgery to remove the tumor followed by observation.
Treatment of newly diagnosed immature teratomas includes the following:
- Surgery to remove the tumor followed by observation for stage I tumors.
- Surgery to remove the tumor for stage I–IV tumors. In young children, surgery is followed by observation; the use of chemotherapy after surgery is controversial. In adolescents and young adults, chemotherapy is given after surgery.
Sometimes a mature or immature teratoma also has malignant cells. A teratoma with malignant cells may need to be treated differently.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Malignant Testicular Germ Cell Tumors
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed malignant testicular germ cell tumors may include the following:
For boys younger than 11 years:
- Surgery (radical inguinal orchiectomy) followed by observation for stage I tumors.
- Surgery (radical inguinal orchiectomy) followed by chemotherapy for stage II–IV tumors and repeat surgery to remove any remaining tumor.
- A clinical trial of a new regimen of surgery followed by observation for stage I tumors or chemotherapy for stage II–IV tumors.
For boys 11 years and older:
Malignant testicular germ cell tumors in boys 11 years and older are treated differently than they are in young boys. For more information, see Testicular Cancer Treatment.
- Surgery to remove the tumor. Sometimes lymph nodes in the abdomen are also removed.
- A clinical trial of a new regimen of surgery followed by observation for stage I tumors or chemotherapy for stage II–IV tumors.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Malignant Ovarian Germ Cell Tumors
In This Section
- Dysgerminomas
- Nongerminomas
Dysgerminomas
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed stage I dysgerminomas of the ovary may include the following:
- Surgery (unilateral salpingo-oophorectomy) followed by observation. Chemotherapy may be given if tumor marker levels do not decrease after surgery or the tumor comes back.
- A clinical trial of a new regimen of surgery followed by observation.
Treatment of newly diagnosed stages II–IV dysgerminomas of the ovary may include the following:
- Surgery (unilateral salpingo-oophorectomy) followed by chemotherapy.
- Chemotherapy to shrink the tumor, followed by surgery (unilateral salpingo-oophorectomy).
Nongerminomas
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed nongerminomas of the ovary, such as yolk sac tumors, mixed germ cell tumors, choriocarcinoma, and embryonal carcinomas, in young girls may include the following:
- Surgery followed by observation for stage I tumors.
- Surgery followed by chemotherapy for stage I–IV tumors.
- A clinical trial of a new regimen of surgery followed by observation for stage I tumors or chemotherapy for stage II–IV.
Treatment of newly diagnosed nongerminomas of the ovary in adolescents and young women may include the following:
- Surgery and chemotherapy for stage I–IV tumors.
- A clinical trial of a new regimen of surgery followed by observation for stage I or chemotherapy for stage II–IV.
Treatment of newly diagnosed nongerminomas of the ovary that cannot be removed by primary surgery without risk to nearby tissue may include the following:
- Biopsy followed by chemotherapy and surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Malignant Extragonadal Extracranial Germ Cell Tumors
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed childhood malignant extragonadal extracranial germ cell tumors in young children may include the following:
- Surgery and chemotherapy for stage I–IV tumors.
- Biopsy followed by chemotherapy with or without surgery for stage III and IV tumors.
In addition to stage of the disease, treatment of malignant extragonadal extracranial germ cell tumors also depends on where the tumor formed in the body:
- For tumors in the sacrum or coccyx, chemotherapy to shrink the tumor followed by surgery to remove the tumor and coccyx.
- For tumors in the mediastinum, chemotherapy before or after surgery to remove the tumor in the mediastinum.
- For tumors in the abdomen, biopsy followed by chemotherapy to shrink the tumor and surgery to remove the tumor in the abdomen.
- For tumors in the head and neck, surgery to remove the tumor in the head or neck, which may be followed by chemotherapy if the tumor is cancer.
Treatment of newly diagnosed childhood malignant extragonadal extracranial germ cell tumors in adolescents and young adults may include the following:
- Surgery.
- Chemotherapy.
- Chemotherapy followed by surgery to remove the tumor.
- A clinical trial of a new regimen of surgery followed by observation for stage I tumors or chemotherapy for stage II–IV tumors.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Childhood Malignant Extracranial Germ Cell Tumors
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent childhood extracranial germ cell tumors may include the following:
- Surgery.
- Chemotherapy given before or after surgery, for most malignant extracranial germ cell tumors including immature teratomas, malignant testicular germ cell tumors, and malignant ovarian germ cell tumors.
- Chemotherapy for recurrent malignant testicular germ cell tumors and recurrent nongerminomas of the ovary that were stage I at diagnosis.
- High-dose chemotherapy and stem cell transplant.
- Radiation therapy followed by surgery to remove cancer that has spread to the brain.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Childhood Cancer
For more information from the National Cancer Institute about childhood extracranial germ cell tumors, see the following:
- Extracranial Germ Cell Tumor (Childhood) Home Page
- Computed Tomography (CT) Scans and Cancer
- Targeted Therapy to Treat Cancer
For more childhood cancer information and other general cancer resources, visit:
- About Cancer
- Childhood Cancers
- CureSearch for Children's Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Cancer Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors, Caregivers, and Advocates
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood extracranial germ cell tumors. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Extracranial Germ Cell Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/extracranial-germ-cell/patient/germ-cell-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389180]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Updated:
Source URL: https://www.cancer.gov/node/2599/syndication
Source Agency: National Cancer Institute (NCI)
Captured Date: 2013-09-14 09:01:05.0