Late Effects of Treatment for Childhood Cancer
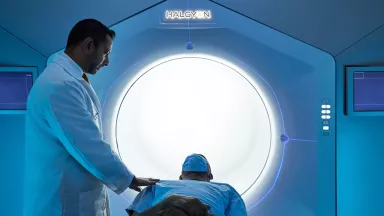
Access care and support for the late effects of treatment for childhood cancer at the Children’s Hospital at Montefiore Einstein (CHAM), where we are here for your child on their entire cancer journey.
Survivors of childhood cancers are often at risk for physical and psychological challenges months or even years after treatment ends. This can be due to the type of cancer they had, their treatment or the impact these had on their mind and spirit.
CHAM is committed to helping children with these late effects of cancer and maximizing their quality of life. Through our Reassessment and Evaluation After Cancer Treatment (REACT) Clinic, our exceptional medical team provides ongoing monitoring and screening tests to identify any concerns early, and, if necessary, ensure your child receives the appropriate treatment and support. The REACT team also offers workshops throughout the year on important topics such as mental health, nutrition, school achievement and more.
When you want only the best for your child, turn to the caring specialists at Montefiore Einstein Comprehensive Cancer Center at CHAM who are passionate about ending cancer and addressing your child’s whole health needs.

Cancer Clinical Trials
- Blood & Bone Marrow Cancers
- Brain, Spine & Central Nervous System Cancers
- Breast Cancer
- Childhood Cancers
- Endocrine System Cancers
- Gastrointestinal (GI) Cancers
- Genitourinary (GU) & Urologic Cancers
- Gynecologic Cancers
- Head & Neck Cancers
- Kaposi Sarcoma & AIDS-Related Cancers
- Lung & Chest Cancers
- Prostate Cancer
- Sarcomas
- Skin Cancer
As an NCI-designated comprehensive cancer center, Montefiore Einstein Comprehensive Cancer Center supports the mission and guidelines of the National Cancer Institute (NCI). The following information about types of cancer, prevention and treatments is provided by the NCI.
Late Effects of Treatment for Childhood Cancer (PDQ®)–Patient Version
General Information About Late Effects
Key Points
- Late effects are health problems that occur months or years after cancer treatment has ended.
- Late effects in childhood cancer survivors affect the body and mind.
- There are three important factors that affect the risk of late effects.
- The chance of having late effects increases over time.
- Regular follow-up care is very important for survivors of childhood cancer.
- Good health habits are also important for survivors of childhood cancer.
Late effects are health problems that occur months or years after cancer treatment has ended.
Cancer treatments may harm the body's organs, tissues, or bones and cause health problems later in life. They may include physical, mental, and social problems and second cancers. These health problems are called late effects.
Treatments that may cause late effects include:
Doctors are studying the late effects caused by cancer treatment. They are working to improve cancer treatments and stop or lessen late effects. While most late effects are not life-threatening, they may cause serious problems that affect health and quality of life.
Late effects in childhood cancer survivors affect the body and mind.
Late effects in childhood cancer survivors may affect:
- organs, tissues, and body function
- growth and development
- mood, feelings, and actions
- thinking, learning, and memory
- social and psychological adjustment
- risk of second cancers
There are three important factors that affect the risk of late effects.
Many childhood cancer survivors will have late effects. The risk of late effects depends on factors related to the tumor, treatment, and patient. These include:
- Cancer-related factors
- type of cancer
- the organs and tissues that were affected by the cancer
- Treatment-related factors
- type of radiation therapy, part of the body treated, and dose
- chemotherapy type, dose, and schedule
- type of surgery
- stem cell transplant
- how the use of two or more treatments at the same time affects the body
- whether transplanted stem cells attack the body's healthy cells, a condition known as chronic graft-versus-host disease
- Patient-related factors
- the childhood cancer survivor's sex
- health problems the childhood cancer survivor had before being diagnosed with cancer or developed during or after treatment
- the age and developmental stage when diagnosed and treated for childhood cancer
- length of time since diagnosis and treatment
- changes in hormone levels
- the ability of healthy tissue affected by cancer treatment to repair itself
- certain changes in the childhood cancer survivor's genes or a family history of cancer or other conditions
- socioeconomic status
- health habits
The chance of having late effects increases over time.
New treatments for childhood cancer have decreased the number of deaths from the primary cancer. Because childhood cancer survivors are living longer, they are having more late effects after cancer treatment. Survivors may not live as long as people who did not have cancer. The most common causes of death in childhood cancer survivors are:
- the primary cancer comes back
- a second (different) primary cancer forms
- heart and lung damage
Studies of the causes of late effects have led to changes in treatment. This has improved the quality of life for cancer survivors and helps prevent illness and death from late effects.
Regular follow-up care is very important for survivors of childhood cancer.
Regular follow-up by health professionals who are trained to find and treat late effects is important for the long-term health of childhood cancer survivors. Follow-up care will be different for each person who has been treated for cancer. The care plan the cancer survivor receives will depend on their general health and health habits, the type of cancer, the type of treatment, genetic factors, and other medical conditions. Follow-up care includes checking for symptoms of late effects and health education on how to prevent or lessen late effects.
It is important that childhood cancer survivors have an exam at least once a year. The exams should be done by a health professional who knows the survivor's risk for late effects and can recognize the early signs of late effects. Blood and imaging tests may also be done.
Long-term follow-up may improve the health and quality of life for cancer survivors. It also helps doctors study the late effects of cancer treatments so that safer therapies for newly diagnosed children may be developed.
Good health habits are also important for survivors of childhood cancer.
The quality of life for cancer survivors may be improved by behaviors that promote health and well-being. These include a healthy diet, exercise, and regular medical and dental check-ups. These self-care behaviors are especially important for cancer survivors because of their risk of health problems related to treatment. Healthy behaviors may make late effects less severe and lower the risk of other diseases.
Avoiding behaviors that are damaging to health is also important. Smoking, excess alcohol use, illegal drug use, not following good sun protection measures, or not being physically active may worsen organ damage related to treatment and may increase the risk of second cancers.
Second Cancers
Key Points
- Childhood cancer survivors have an increased risk of a second cancer later in life.
- Certain genetic patterns or syndromes may increase the risk of a second cancer.
- People who have been treated for cancer need regular screening tests to check for a second cancer.
- The kind of test used to screen for a second cancer depends in part on the kind of cancer treatment the survivors had in the past.
Childhood cancer survivors have an increased risk of a second cancer later in life.
A different primary cancer that occurs at least two months after cancer treatment ends is called a second cancer. A second cancer may occur months or years after treatment is completed. The type of second cancer that occurs depends in part on the original type of cancer and the cancer treatment. Benign tumors (not cancer) may also occur.
Second cancers that may occur after cancer treatment include:
Myelodysplastic syndrome and acute myeloid leukemia may appear less than 10 years after a primary cancer diagnosis of Hodgkin lymphoma, acute lymphoblastic leukemia, sarcoma, central nervous system (CNS) tumor, non-Hodgkin lymphoma, neuroblastoma, or Wilms tumor and treatment with chemotherapy that included:
- an alkylating agent, such as cyclophosphamide, ifosfamide, mechlorethamine, melphalan, busulfan, carmustine, lomustine, chlorambucil, or dacarbazine
- a topoisomerase II inhibitor agent, such as etoposide
Children treated with radiation to the bone marrow without chemotherapy may also have an increased risk of second acute myeloid leukemia.
Solid tumors that may appear more than 10 years after a primary cancer diagnosis and treatment include:
- Breast cancer. Survivors of childhood, adolescent, and young adult cancers who received high-dose radiation therapy to the chest have an increased risk of developing breast cancer. Certain chemotherapy drugs, including alkylating agents and anthracyclines, also increase a person's risk of breast cancer. Risk is highest for female survivors of Hodgkin lymphoma, sarcoma, and leukemia.
- Thyroid cancer. Thyroid cancer may occur after radiation therapy to the neck for Hodgkin lymphoma, acute lymphoblastic leukemia, or brain tumors; after radioactive iodine therapy for neuroblastoma; after total-body irradiation as part of a stem cell transplant; or after chemotherapy alone.
- Brain tumors. Brain tumors may occur after radiation therapy to the head and/or intrathecal chemotherapy using methotrexate for a primary brain tumor or for cancer that has spread to the brain or spinal cord, such as acute lymphocytic leukemia or non-Hodgkin lymphoma. When intrathecal chemotherapy using methotrexate and radiation treatment are given together, the risk of a brain tumor is even higher.
- Bone and soft tissue tumors. There is an increased risk of bone and soft tissue tumors after radiation treatment for hereditary retinoblastoma, Ewing sarcoma, and other cancers of the bone, with risks increasing at higher doses. Chemotherapy with anthracyclines or alkylating agents also increases the risk of bone and soft tissue tumors, with risk increasing at higher doses.
- Lung cancer. There is an increased risk of lung cancer after radiation treatment to the chest for Hodgkin lymphoma or bone cancer, especially in patients who smoke.
- Stomach, liver, or colorectal cancer. Stomach, liver, or colorectal cancer may occur after receiving radiation therapy to the abdomen or pelvis, chemotherapy, or both. Survivors of Wilms tumor and Hodgkin lymphoma have the highest risk of these second cancers. The risk increases with higher doses of radiation. There is also an increased risk of colorectal polyps.
- Nonmelanoma skin cancer (basal cell carcinoma or squamous cell carcinoma). There is an increased risk of nonmelanoma skin cancer after radiation treatment, and it usually appears in the area where radiation was given. Being exposed to UV radiation may increase this risk. Patients who develop nonmelanoma skin cancer after radiation treatment have an increased chance of developing other types of cancers in the future. The risk of basal cell carcinoma is also increased after treatment with chemotherapy drugs, such as vincristine and vinblastine (called vinca alkaloids). Survivors of hereditary retinoblastoma may have an increased risk of developing nonmelanoma skin cancer.
- Malignant melanoma. Malignant melanoma may occur after radiation or combination chemotherapy with alkylating agents and antimitotic drugs (such as vincristine and vinblastine). Survivors of Hodgkin lymphoma, hereditary retinoblastoma, soft tissue sarcoma, and gonadal tumors are more likely to be at a higher risk of having malignant melanoma. Malignant melanoma as a second cancer is less common than nonmelanoma skin cancer. Survivors of hereditary retinoblastoma may have an increased risk of developing melanoma.
- Oral, laryngeal, and salivary gland cancer. Oral cancer may occur after stem cell transplant with a history of chronic graft-versus-host disease, radiation therapy, or chemotherapy. Survivors of leukemia, osteosarcoma, Hodgkin lymphoma, and soft tissue sarcoma have the highest risk of oral cancers. Childhood, adolescent, and young adult cancer survivors may also be at increased risk of developing oral cancers related to infection with human papillomavirus.
- Kidney cancer. There is an increased risk of kidney cancer after treatment for neuroblastoma, radiation treatment to the middle of the back, or chemotherapy such as cisplatin or carboplatin.
- Bladder cancer and genital cancer. Bladder cancer may occur after chemotherapy with cyclophosphamide. Survivors of heritable retinoblastoma have an increased risk of developing bladder cancer. Female survivors have an increased risk of cancer in the uterus or vulva.
Certain genetic patterns or syndromes may increase the risk of a second cancer.
Some childhood cancer survivors may have an increased risk of developing a second cancer because they have a family history of cancer, an inherited cancer syndrome such as Li-Fraumeni syndrome, or a genetic mutation such as neurofibromatosis type 1. Problems with the way DNA is repaired in cells and the way anticancer drugs are used by the body may also affect the risk of second cancers.
People who have been treated for cancer need regular screening tests to check for a second cancer.
It is important for people who have been treated for cancer to be checked for a second cancer before symptoms appear. This is called screening and may help find a second cancer when it is smaller and has not spread. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
It is important to remember that the doctor does not necessarily think a childhood cancer survivor has cancer if he or she suggests a screening test. Screening tests are given when the cancer survivor has no cancer symptoms. If a screening test result is abnormal, more tests may be done to find out if there is a second cancer. These are called diagnostic tests.
The kind of test used to screen for a second cancer depends in part on the kind of cancer treatment the survivors had in the past.
Childhood cancer survivors should have a physical exam and medical history done once a year. A physical exam of the body is done to see how healthy the person is and to check for signs of disease, such as lumps, changes in the skin, or anything else that seems unusual. A medical history is taken to learn about the cancer survivor's health habits and past illnesses and treatments.
Childhood cancer survivors who received radiation therapy may have the following tests and procedures to check for skin, breast, or colorectal cancer:
- Skin exam is when a doctor or nurse checks the skin for bumps or spots that look abnormal in color, size, shape, or texture, especially in the area where radiation was given. It is suggested that a skin exam be done once a year to check for signs of skin cancer. The doctor will also provide information about sun protection behaviors to reduce the risk of skin cancer.
- Breast self-exam is an exam of the breast by the patient. The patient carefully feels the breasts and under the arms for lumps or anything else that seems unusual. It is suggested that women treated with a higher dose of radiation therapy to the chest do a monthly breast self-exam beginning at puberty. Talk to the doctor about when breast self-exams should begin.
- Clinical breast exam (CBE) is an exam of the breast by a doctor or other health professional. The doctor will carefully feel the breasts and under the arms for lumps or anything else that seems unusual. It is suggested that women treated with a higher dose of radiation therapy to the chest have a clinical breast exam every year beginning at puberty until age 25. After age 25 or 8 years after radiation treatments end (whichever is first), clinical breast exams are done every 6 months. Talk to the doctor about when clinical breast exams should begin.
- Mammogram is an x-ray of the breast. A mammogram may be done in women who had a higher dose of radiation to the chest and who do not have dense breasts. It is suggested that these women have a mammogram once a year starting 8 years after treatment or at age 25, whichever is later. Talk to the doctor about when mammograms to check for breast cancer should begin.
- Breast MRI (magnetic resonance imaging) uses a magnet, radio waves, and a computer to make a series of detailed pictures of the breast. This procedure is also called nuclear magnetic resonance imaging (NMRI). An MRI may be done in women who had a higher dose of radiation to the chest and who have dense breasts. It is suggested that these women have an MRI once a year starting 8 years after treatment or at age 25, whichever is later. Talk to the doctor about whether an MRI of the breast to check for breast cancer is needed.
- Colonoscopy is a procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope is inserted through the rectum into the colon. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer. It is suggested that childhood cancer survivors who had a higher dose of radiation to the abdomen, pelvis, or spine have a colonoscopy every 5 years. This begins at age 30 or 5 years after treatment ended, whichever is later. Talk to your doctor about when colonoscopies to check for colorectal cancer should begin.
- Multitarget stool DNA test is a test to collect stool to check for cancer cells. This test may be done every 3 years beginning at age 30 or 5 years after treatment ended.
Cardiovascular System
Key Points
- Heart and blood vessel late effects are more likely to occur after treatment for certain childhood cancers.
- Radiation to the chest and certain types of chemotherapy increase the risk of heart and blood vessel late effects.
- Late effects that affect the heart and blood vessels may cause certain health problems.
- Possible symptoms of heart and blood vessel late effects include trouble breathing and chest pain.
- Certain tests and procedures are used to diagnose health problems in the heart and blood vessels.
- Health habits that promote a healthy heart and blood vessels are important for survivors of childhood cancer.
Heart and blood vessel late effects are more likely to occur after treatment for certain childhood cancers.
Cardiovascular disease occurs at a younger age in childhood cancer survivors. Treatment for these and other childhood cancers may cause heart and blood vessel late effects:
- acute lymphoblastic leukemia (ALL)
- acute myeloid leukemia (AML)
- brain and spinal cord tumors
- head and neck cancers
- Hodgkin lymphoma
- non-Hodgkin lymphoma
- osteosarcoma
- Wilms tumor
- cancers treated with a stem cell transplant
Radiation to the chest and certain types of chemotherapy increase the risk of heart and blood vessel late effects.
The risk of health problems involving the heart and blood vessels increases after treatment with:
- Radiation to the chest, spine, brain, neck, kidneys, or total-body irradiation (TBI) as part of a stem cell transplant. The risk of problems depends on the area of the body that was exposed to radiation, the amount of radiation given, and whether the radiation was given in small or large doses.
- Certain types of chemotherapy. Chemotherapy with anthracyclines such as doxorubicin, daunorubicin, idarubicin, and epirubicin, and with anthraquinones such as mitoxantrone increase the risk of heart and blood vessel problems. The risk of problems depends on the total dose of chemotherapy given and the type of drug used. It also depends on whether treatment with anthracyclines was given to a child younger than 13 years and whether a drug called dexrazoxane was given during treatment with anthracyclines. Dexrazoxane may lessen heart and blood vessel damage up to 5 years after treatment. Ifosfamide, cyclophosphamide, methotrexate, asparaginase, and chemotherapy with a platinum, such as carboplatin and cisplatin, may also cause heart and blood vessel late effects.
- Stem cell transplant.
- Nephrectomy (surgery to remove all or part of a kidney).
Childhood cancer survivors who were treated with both radiation therapy to the heart or blood vessels and certain types of chemotherapy are at greatest risk.
Other factors that may also increase the risk of heart and blood vessel late effects include:
- Longer time since treatment.
- Having high blood pressure or other risk factors for heart disease, such as a family history of heart disease, having excess body weight, smoking, high cholesterol, or diabetes. When these risk factors are combined, the risk of late effects is even higher.
- Having lower than normal amounts of thyroid, growth, or sex hormones.
New treatments that decrease the amount of radiation given, use lower doses of chemotherapy or less harmful chemotherapy drugs, and incorporate dexrazoxane may be leading to a lower risk of heart and blood vessel late effects in childhood cancer survivors.
Late effects that affect the heart and blood vessels may cause certain health problems.
Childhood cancer survivors who received radiation or certain types of chemotherapy have an increased risk of late effects to the heart and blood vessels and related health problems. These include:
- abnormal heartbeat
- weakened heart muscle
- inflamed heart or sac around the heart
- damage to the heart valves
- hardening of the heart arteries (coronary artery disease)
- congestive heart failure
- high blood pressure
- chest pain or heart attack
- blood clots or one or more strokes
- carotid artery disease
Possible symptoms of heart and blood vessel late effects include trouble breathing and chest pain.
These and other symptoms may be caused by heart and blood vessel late effects or by other problems:
- trouble breathing, especially when lying down
- heartbeat that is too slow, too fast, or different from the heart's normal rhythm
- chest pain or pain in the arm or leg
- swelling of the feet, ankles, legs, or abdomen
- when exposed to cold or having strong emotions, the fingers, toes, ears, or nose become white and then turn blue, and sometimes the fingers will also have pain or tingling
- sudden numbness or weakness of the face, arm, or leg (especially on one side of the body)
- sudden confusion or trouble speaking or understanding speech
- sudden trouble seeing with one or both eyes
- sudden trouble walking or feeling dizzy
- sudden loss of balance or coordination
- sudden severe headache for no known reason
- pain, warmth, or redness in one area of the arm or leg, especially the back of the lower leg
The only way to know if these symptoms are caused by heart and blood vessel late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the heart and blood vessels.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Electrocardiogram (EKG) is a recording of the heart's electrical activity to check its rate and rhythm. A number of small pads (electrodes) are placed on the patient's chest, arms, and legs, and are connected by wires to the EKG machine. Heart activity is then recorded as a line graph on paper. Electrical activity that is faster or slower than normal may be a sign of heart disease or damage.
- Echocardiogram is a procedure in which high-energy sound waves (ultrasound) are bounced off the heart and nearby tissues or organs and make echoes. A moving picture is made of the heart and heart valves as blood is pumped through the heart.
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs such as the heart and make echoes. The echoes form a picture of body tissues called a sonogram.
- Magnetic resonance imaging (MRI) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). This procedure is done to check for blood clots.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is done to check for blood clots. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
- Magnetic resonance angiography (MRA) uses radio waves and a powerful magnet linked to a computer to create detailed pictures of the blood vessels and blood flow inside the body. A dye may be injected into a vein to make the blood vessels and blood flow easier to see. This may be used to check for blood clots or other blood vessel problems.
- Lipid profile studies use a blood sample to measure the amounts of triglycerides, cholesterol, and low- and high-density lipoprotein cholesterol in the blood.
Talk to the doctor about whether tests and procedures are needed to check for signs of heart and blood vessel late effects. If tests are needed, find out how often they should be done.
Health habits that promote a healthy heart and blood vessels are important for survivors of childhood cancer.
Childhood cancer survivors may lower their risk of heart and blood vessel late effects by having a healthy lifestyle, which includes:
- a healthy weight
- a heart-healthy diet, high in vegetables, fruits, whole grains, fish, and poultry, and low in red or processed meats
- regular exercise
- not smoking
Central Nervous System
Key Points
- Brain and spinal cord late effects are more likely to occur after treatment of brain tumors and acute lymphoblastic leukemia.
- Radiation to the brain increases the risk of brain and spinal cord late effects.
- Late effects that affect the brain and spinal cord may cause certain health problems.
- Possible symptoms of brain and spinal cord late effects include headaches, loss of coordination, and seizures.
- Certain tests and procedures are used to diagnose health problems in the brain and spinal cord.
- Survivors of childhood cancer have an increased risk of mental health disorders.
- Some childhood cancer survivors have post-traumatic stress disorder.
- Adolescents who are diagnosed with cancer may have social problems later in life.
Brain and spinal cord late effects are more likely to occur after treatment of brain tumors and acute lymphoblastic leukemia.
Treatment for these and other childhood cancers may cause brain and spinal cord late effects:
- acute lymphoblastic leukemia (ALL)
- acute myeloid leukemia (AML)
- brain and spinal cord tumors
- head and neck cancers, including retinoblastoma
- Hodgkin lymphoma
- non-Hodgkin lymphoma
- osteosarcoma
- soft tissue sarcoma
- neuroblastoma
- Wilms tumor
- cancers treated with a stem cell transplant
Radiation to the brain increases the risk of brain and spinal cord late effects.
The risk of health problems that affect the brain or spinal cord increases after treatment with:
- radiation (especially high doses) to the brain or spinal cord or total-body irradiation given as part of a stem cell transplant
- intrathecal or intraventricular chemotherapy
- chemotherapy with high-dose methotrexate or cytarabine that can cross the blood-brain barrier (protective lining around the brain) or high-dose chemotherapy given as part of a stem cell transplant
- surgery to remove a tumor on the brain or spinal cord
When radiation to the brain and intrathecal chemotherapy are given at the same time, the risk of late effects is higher.
The following may also increase the risk of brain and spinal cord late effects in childhood brain tumor survivors:
- where the tumor formed in the brain and spinal cord
- being 5 years old or younger at the time of treatment
- being female
- having hydrocephalus and a shunt placed to remove the extra fluid from the ventricles
- having hearing loss
- having cerebellar mutism following surgery to remove the brain tumor
- having a personal history of stroke
- seizures
- socioeconomic status
Late effects that affect the brain and spinal cord may cause certain health problems.
Childhood cancer survivors who received radiation, certain types of chemotherapy, or surgery to the brain or spinal cord have an increased risk of late effects to the brain and spinal cord and related health problems. A child may develop these problems soon after treatment or years later in adulthood. Brain and spinal cord late effects include:
- headaches that may go away after vomiting
- loss of balance, lack of coordination, or trouble walking
- dizziness
- seizures
- loss of the myelin sheath that covers nerve fibers in the brain
- movement disorders that affect the legs and eyes or the ability to speak and swallow
- nerve damage in the hands or feet
- stroke, with an increased risk for a second stroke for survivors who received radiation to the brain, have a history of high blood pressure, or were older than 40 years when they had their first stroke
- a small amount of bleeding in the brain (brain microbleeds)
- daytime sleepiness
- hydrocephalus
- loss of bladder and/or bowel control
- clusters of abnormal blood vessels (cavernomas)
- back pain
Survivors may also have late effects that affect thinking, learning, memory, emotions, and behavior.
New ways of using more targeted and lower doses of radiation to the brain may lessen the risk of brain and spinal cord late effects.
Possible symptoms of brain and spinal cord late effects include headaches, loss of coordination, and seizures.
These symptoms may be caused by brain and spinal cord late effects or by other problems:
- trouble speaking or swallowing
- trouble with having the eyes work together
- numbness, tingling, or weakness in the hands or feet
- being unable to bend the ankle to lift the foot up
- sudden numbness or weakness of the face, arm, or leg (especially on one side of the body)
- unusual sleepiness or change in activity level
- unusual changes in personality or behavior
- a change in bowel habits or trouble urinating
- increase in head size (in infants)
- sudden confusion or trouble speaking or understanding speech
- sudden trouble seeing with one or both eyes
- sudden severe headache for no known reason
Other symptoms include:
- problems with memory
- problems with paying attention
- trouble with solving problems
- trouble with organizing thoughts and tasks
- slower ability to learn and use new information
- trouble learning to read, write, or do math
- trouble coordinating movement between the eyes, hands, and other muscles
- delays in normal development
- social withdrawal or trouble getting along with others
The only way to know if these symptoms are caused by brain and spinal cord late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the brain and spinal cord.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Neurological exam is a series of questions and tests to check the brain, spinal cord, and nerve function. The exam checks a person's mental status, coordination, and ability to walk normally, and how well the muscles, senses, and reflexes work. This may also be called a neuro exam or a neurologic exam. In some cases, a more complete exam may be done by a neurologist or neurosurgeon.
- Neuropsychological assessment is a series of tests to examine the patient's mental processes and behavior. Areas that are checked usually include:
- knowing who and where you are and what day it is
- ability to learn and remember new information
- intelligence
- ability to solve problems
- use of spoken and written language
- eye-hand coordination
- ability to organize information and tasks
Talk to the doctor about whether tests and procedures are needed to check for signs of brain and spinal cord late effects. If tests are needed, find out how often they should be done.
Survivors of childhood cancer have an increased risk of mental health disorders.
Survivors of childhood cancer are more likely to be diagnosed with mental health disorders than their peers who have not had cancer. These disorders include:
- depression
- anxiety
- autism spectrum disorder
- bipolar disorder
- obsessive-compulsive disorder
- post-traumatic stress disorder
Having a mental health disorder may cause problems with personal relationships, education, employment, and health, and cause thoughts of suicide. As a result, survivors may be less likely to live on their own as adults.
Follow-up care for childhood cancer survivors should include screening and treatment for possible psychological distress or mental health disorders.
For more information about psychological distress and coping skills for people with cancer, see:
Some childhood cancer survivors have post-traumatic stress disorder.
Being diagnosed and treated for a life-threatening disease may be traumatic. This trauma may cause post-traumatic stress disorder (PTSD). PTSD is defined as having certain behaviors following a stressful event that involved death or the threat of death, serious injury, or a threat to oneself or others.
PTSD can affect cancer survivors in the following ways:
- constantly reliving or thinking about the time they were diagnosed and treated for cancer
- having nightmares or flashbacks
- avoiding places, events, and people that remind them of the cancer experience
In general, childhood cancer survivors show low levels of PTSD, depending in part on their coping style and the coping style of their parents. Survivors who received radiation therapy to the head when younger than 4 years or survivors who received intensive treatment may be at higher risk of PTSD. Family problems, little or no social support from family or friends, and stress not related to the cancer may increase the chances of having PTSD.
Because avoiding places and people connected to the cancer may be part of PTSD, survivors with PTSD may not get the medical treatment they need.
Adolescents who are diagnosed with cancer may have social problems later in life.
Adolescents who are diagnosed with cancer may reach fewer social milestones or reach them later in life than adolescents not diagnosed with cancer. Social milestones include having a first boyfriend or girlfriend, getting married, and having a child. They may also have trouble getting along with other people or feel like they are not liked by others their age.
Cancer survivors in this age group have reported being less satisfied with their health and their lives in general compared with others of the same age who did not have cancer. Adolescents and young adults who survived cancer need special programs that give psychological, educational, and job support.
Digestive System
Key Points
- Teeth and jaws
- Problems with the teeth and jaws are more likely to occur after treatment for certain childhood cancers.
- Radiation to the head and neck and certain types of chemotherapy increase the risk of late effects to the teeth and jaws.
- Late effects that affect the teeth and jaws may cause certain health problems.
- Possible symptoms of late effects of the teeth and jaws include tooth decay (cavities) and jaw pain.
- Certain tests and procedures are used to diagnose health problems in the mouth and jaws.
- Regular dental care is very important for survivors of childhood cancer.
- Digestive tract
- Digestive tract late effects are more likely to occur after treatment for certain childhood cancers.
- Radiation to the bladder, prostate, or testicles and certain types of chemotherapy increase the risk of digestive tract late effects.
- Late effects that affect the digestive tract may cause certain health problems.
- Possible symptoms of digestive tract late effects include abdominal pain and diarrhea.
- Certain tests and procedures are used to diagnose health problems in the digestive tract.
- Liver and bile ducts
- Liver and bile duct late effects are more likely to occur after treatment for certain childhood cancers.
- Certain types of chemotherapy and radiation to the liver or bile ducts increase the risk of late effects.
- Late effects that affect the liver and bile ducts may cause certain health problems.
- Possible symptoms of liver and bile duct late effects include abdominal pain and jaundice.
- Certain tests and procedures are used to diagnose health problems in the liver and bile duct.
- Health habits that promote a healthy liver are important for survivors of childhood cancer.
- Pancreas
- Radiation therapy increases the risk of pancreatic late effects.
- Late effects that affect the pancreas may cause certain health problems.
- Possible symptoms of pancreatic late effects include frequent urination and being thirsty.
- Certain tests and procedures are used to diagnose health problems in the pancreas.
Treatment with chemotherapy, radiation therapy, or surgery may cause problems throughout the digestive system, which starts at the mouth and ends at the rectum.
Teeth and jaws
Problems with the teeth and jaws are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause late effects of the teeth and jaws:
- head and neck cancers
- Hodgkin lymphoma
- neuroblastoma
- leukemia that spreads to the brain and spinal cord
- nasopharyngeal cancer
- brain tumors
- cancers treated with total-body irradiation (TBI) as part of a stem cell transplant
Radiation to the head and neck and certain types of chemotherapy increase the risk of late effects to the teeth and jaws.
The risk of health problems that affect the teeth and jaws increases after treatment with:
- radiation therapy to the head and neck
- TBI as part of a stem cell transplant
- chemotherapy, especially with higher doses of alkylating agents such as cyclophosphamide
- surgery in the head and neck area
Risk is also increased in survivors who were younger than 5 years at the time of treatment because their permanent teeth had not fully formed.
Late effects that affect the teeth and jaws may cause certain health problems.
Teeth and jaws late effects and related health problems include:
- teeth that are not normal
- tooth decay (including cavities) and gum disease
- salivary glands that do not make enough saliva
- death of the bone cells in the jaw
- changes in the way the face, jaw, or skull form
- a second cancer in the mouth
Possible symptoms of late effects of the teeth and jaws include tooth decay (cavities) and jaw pain.
These and other symptoms may be caused by late effects of the teeth and jaws or by other problems:
- teeth are small or do not have a normal shape
- missing permanent teeth
- permanent teeth come in at a later than normal age
- teeth have less enamel than normal
- more tooth decay (cavities) and gum disease than normal
- dry mouth
- trouble chewing, swallowing, and speaking
- jaw pain
- jaws do not open and close the way they should
The only way to know if these symptoms are caused by late effects of the teeth and jaws is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the mouth and jaws.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Dental exam is an exam of the teeth, mouth, and jaws to check general signs of dental health, including checking for signs of disease, such as cavities or anything that seems unusual. This may also be called a dental check-up.
- Panorex x-ray is an x-ray of all of the teeth and their roots. An x-ray is a type of radiation that can go through the body and make pictures.
- X-ray of the jaws is an x-ray of the jaws. An x-ray is a type of radiation that can go through the body and make pictures.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the head and neck. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
- Magnetic resonance imaging (MRI) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the head and neck. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Biopsy is a procedure in which a sample of tissue is removed from the tumor so that a pathologist can view it under a microscope to check for signs of cancer.
Talk to the doctor about whether tests and procedures are needed to check for signs of teeth and jaw late effects. If tests are needed, find out how often they should be done.
Regular dental care is very important for survivors of childhood cancer.
Doctors suggest that survivors of childhood cancer have a dental check-up and a cleaning and fluoride treatment every 6 months. Children who had radiation therapy to the oral cavity may also see an orthodontist or an otolaryngologist. If lesions are present in the mouth, a biopsy may be needed.
Digestive tract
Digestive tract late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause late effects of the digestive tract (esophagus, stomach, small and large intestines, rectum and anus):
- germ cell tumors
- Hodgkin lymphoma
- non-Hodgkin lymphoma
- neuroblastoma
- rhabdomyosarcoma of the bladder or prostate, or near the testicles
- Wilms tumor
Radiation to the bladder, prostate, or testicles and certain types of chemotherapy increase the risk of digestive tract late effects.
The risk of health problems that affect the digestive tract increases after treatment with:
- Radiation therapy to the abdomen or areas near the abdomen, such as the esophagus, bladder, prostate, or testicles, may cause digestive tract problems that begin quickly and last for a short time. In some patients, however, digestive tract problems are delayed and long-lasting. These late effects are caused by radiation therapy that damages the blood vessels. Receiving higher doses of radiation therapy or receiving chemotherapy such as dactinomycin or anthracyclines together with radiation therapy may increase this risk.
- Abdominal surgery or pelvic surgery to remove the bladder.
- Chemotherapy with alkylating agents such as cyclophosphamide, procarbazine, and ifosfamide, or with anthracyclines such as doxorubicin, daunorubicin, idarubicin, and epirubicin.
- Stem cell transplant.
The following may also increase the risk of digestive tract late effects:
- older age at diagnosis or when treatment begins
- treatment with both radiation therapy and chemotherapy
- a history of chronic graft-versus-host disease
Late effects that affect the digestive tract may cause certain health problems.
Digestive tract late effects and related health problems include:
- a narrowing of the esophagus or intestine
- the muscles of the esophagus do not work well
- reflux
- diarrhea, constipation, fecal incontinence, or blocked bowel
- bowel perforation (a hole in the intestine)
- inflammation of the intestines
- death of part of the intestine
- intestine is not able to absorb nutrients from food
- a second cancer
Possible symptoms of digestive tract late effects include abdominal pain and diarrhea.
These and other symptoms may be caused by digestive tract late effects or by other problems:
- trouble swallowing or feeling like food is stuck in the throat
- heartburn
- fever with severe pain in the abdomen and nausea
- pain in the abdomen
- a change in bowel habits (constipation or diarrhea)
- nausea and vomiting
- frequent gas pains, bloating, fullness, or cramps
- reflux
The only way to know if these symptoms are caused by digestive late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the digestive tract.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Digital rectal exam is an exam where the doctor or nurse inserts a lubricated, gloved finger into the rectum to feel for lumps or anything else that seems unusual.
- Blood chemistry studies is a test that uses a blood sample to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
- Kidney, ureter, and bladder x-ray is a type of radiation that can go through the body and make pictures of the abdomen, kidney, ureter, or bladder to check for signs of disease.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
- Magnetic resonance imaging (MRI) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Barium swallow is a series of x-rays of the throat, esophagus, stomach, and the first part of the small intestine (duodenum). For this procedure, the patient drinks a liquid that contains barium (a silver-white metallic compound). The barium coats the esophagus and stomach which helps them show up more clearly in x-rays. This procedure is also called an upper GI series.
Talk to the doctor about whether tests and procedures are needed to check for signs of digestive tract late effects. If tests are needed, find out how often they should be done.
Liver and bile ducts
Liver and bile duct late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause liver or bile duct late effects:
- acute lymphoblastic leukemia (ALL)
- liver cancer
- Wilms tumor
- cancers treated with a stem cell transplant
Certain types of chemotherapy and radiation to the liver or bile ducts increase the risk of late effects.
The risk of liver or bile duct late effects may be increased in childhood cancer survivors treated with:
- surgery to remove part of the liver or a liver transplant
- chemotherapy that includes high-dose cyclophosphamide as part of a stem cell transplant
- chemotherapy such as 6-mercaptopurine, 6-thioguanine, methotrexate, and dactinomycin
- radiation therapy to the liver and bile ducts, with the risk depending on:
- the dose of radiation and how much of the liver is treated
- age when treated (the younger the age, the higher the risk)
- whether there was surgery to remove part of the liver
- whether chemotherapy, such as doxorubicin or dactinomycin, was given together with radiation therapy
- stem cell transplant
The following may also increase the risk of liver and bile duct late effects:
- hepatitis B or hepatitis C infection
- history of chronic graft-versus-host disease
- liver damage caused by veno-occlusive disease/sinusoidal obstruction syndrome
- tissue and organ damage from the buildup of extra iron after having many blood transfusions
Late effects that affect the liver and bile ducts may cause certain health problems.
Liver and bile duct late effects and related health problems include:
- liver dysfunction
- gallstones
- benign liver lesions
- an overgrowth of connective tissue in the liver (liver fibrosis) or cirrhosis
- fatty liver with insulin resistance (a condition in which the body makes insulin but cannot use it well)
Possible symptoms of liver and bile duct late effects include abdominal pain and jaundice.
These and other symptoms may be caused by liver and bile duct late effects or by other problems:
- weight gain or weight loss
- swelling of the abdomen
- nausea and vomiting
- pain in the abdomen that may occur near the ribs, often on the right side after eating a fatty meal
- yellowing of the skin and whites of the eyes (jaundice)
- light-colored bowel movements
- diarrhea
- dark-colored urine
- a lot of gas
- lack of appetite
- feeling tired or weak
The only way to know if these symptoms are caused by liver and bile duct late effects is to see a doctor.
Sometimes there are no signs or symptoms of liver or bile duct late effects and treatment may not be needed.
Certain tests and procedures are used to diagnose health problems in the liver and bile duct.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry studies use a blood sample to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease. For example, there may be a higher level of bilirubin, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) in the body if the liver has been damaged.
- Ferritin level uses a blood sample to measure the amount of ferritin. Ferritin is a protein that binds to iron and stores it for use by the body. After a stem cell transplant, a high ferritin level may be a sign of liver disease.
- Complete blood count (CBC) is when a sample of blood is drawn and checked for:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
This test is used to check the amount of platelets in the body.
- Prothrombin time (PT) test measures how long it takes for the blood to clot.
- Hepatitis assay uses a blood sample to check for pieces of the hepatitis virus. The blood sample may also be used to measure how much hepatitis virus is in the blood. All patients who had a blood transfusion before 1972 should have a screening test for hepatitis B. Patients who had a blood transfusion before 1993 should have a screening test for hepatitis C.
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs, such as the gall bladder, and make echoes. The echoes form a picture of body tissues called a sonogram.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs and tissue show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
- Magnetic resonance imaging (MRI) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Talk to the doctor about whether tests and procedures are needed to check for signs of liver or bile duct late effects. If tests are needed, find out how often they should be done.
Health habits that promote a healthy liver are important for survivors of childhood cancer.
Childhood cancer survivors with liver late effects should take care to protect their health, including:
- having a healthy weight
- not drinking alcohol
- getting vaccines for hepatitis A and hepatitis B viruses
Pancreas
Radiation therapy increases the risk of pancreatic late effects.
The risk of pancreatic late effects may be increased in childhood cancer survivors after treatment with:
- radiation therapy to the abdomen
- total-body irradiation as part of a stem cell transplant
Late effects that affect the pancreas may cause certain health problems.
Pancreatic late effects and related health problems include:
- Insulin resistance is a condition in which the body does not use insulin the way it should. Insulin is needed to help control the amount of glucose (a type of sugar) in the body. Because the insulin does not work the way it should, glucose and fat levels rise.
- Diabetes mellitus is a disease in which the body does not make enough insulin or does not use it the way it should. When there is not enough insulin, the amount of glucose in the blood increases and the kidneys make a large amount of urine. Survivors also have an increased risk of prediabetes, which can lead to diabetes.
Possible symptoms of pancreatic late effects include frequent urination and being thirsty.
These and other symptoms may be caused by pancreatic late effects or by other problems:
- frequent urination
- feeling very thirsty
- feeling very hungry
- weight loss for no known reason
- feeling very tired
- frequent infections, especially of the skin, gums, or bladder
- blurred vision
- cuts or bruises that are slow to heal
- numbness or tingling in the hands or feet
The only way to know if these symptoms are caused by pancreatic late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the pancreas.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Glycated hemoglobin (A1C) test uses a sample of blood to measure the amount of glucose that is attached to red blood cells. A higher-than-normal amount of glucose attached to red blood cells can be a sign of diabetes mellitus.
- Fasting blood sugar test uses a blood sample to measure the amount of glucose in the blood. This test is done after the patient has had nothing to eat overnight. A higher-than-normal amount of glucose in the blood can be a sign of diabetes mellitus.
Endocrine System
Key Points
- Thyroid gland
- Thyroid late effects are more likely to occur after treatment for certain childhood cancers.
- Radiation therapy to the head and neck increases the risk of thyroid late effects.
- Late effects that affect the thyroid may cause certain health problems.
- Symptoms of thyroid late effects depend on whether there is too little or too much thyroid hormone in the body.
- Certain tests and procedures are used to diagnose health problems in the thyroid.
- Hypothalamus and pituitary gland
- Neuroendocrine late effects may be caused after treatment for certain childhood cancers.
- Treatment that affects the hypothalamus or pituitary gland increases the risk of neuroendocrine system late effects.
- Late effects that affect the hypothalamus may cause certain health problems.
- Certain tests and procedures are used to diagnose health problems in the neuroendocrine system.
- Metabolic syndrome
- Metabolic syndrome is more likely to occur after treatment for certain childhood cancers.
- Radiation therapy increases the risk of metabolic syndrome.
- Certain tests and procedures are used to diagnose metabolic syndrome.
- Metabolic syndrome may cause heart and blood vessel disease and diabetes.
- Weight changes and frailty
- Weight changes and frailty are late effects that are more likely to occur after treatment for certain childhood cancers.
- Radiation therapy increases the risk of weight changes and frailty.
- Certain tests and procedures are used to diagnose a change in weight.
Thyroid gland
Thyroid late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause thyroid late effects:
- acute lymphoblastic leukemia (ALL)
- brain tumors
- head and neck cancers
- Hodgkin lymphoma
- neuroblastoma
- cancers treated with a stem cell transplant
Radiation therapy to the head and neck increases the risk of thyroid late effects.
The risk of thyroid late effects may be increased in childhood cancer survivors after treatment with:
- radiation therapy to the thyroid as part of radiation therapy to the head and neck or to the pituitary gland in the brain
- total-body irradiation or chemotherapy as part of a stem cell transplant
- MIBG (radioactive iodine) therapy for neuroblastoma
- chemotherapy such as alkylating agents, anthracyclines, or bleomycin
- surgery to remove part of the thyroid
The risk also is increased in females, in survivors who were a young age at the time of treatment, in survivors who had a higher radiation dose, and as the time since diagnosis and treatment gets longer. Risk for endocrine problems also depends on the location of the tumor.
Late effects that affect the thyroid may cause certain health problems.
Thyroid late effects and related health problems include:
- Hypothyroidism (not enough thyroid hormone): There is a higher risk of hypothyroidism in survivors treated with head and neck radiation involving the thyroid gland, especially survivors of Hodgkin lymphoma. This is the most common thyroid late effect. It usually occurs 2 to 5 years after treatment ends but may occur more than 25 years after radiation therapy. It is more common in girls than boys. Children, adolescents, and young adults treated with proton beam radiation therapy may have a lower risk of developing hypothyroidism.
- Hyperthyroidism (too much thyroid hormone): The risk of hyperthyroidism increases with higher doses of radiation therapy to the thyroid gland. Hyperthyroidism is less common than hypothyroidism. It usually occurs 5 years after treatment ends, but may occur more than 25 years after radiation therapy.
- Lumps in the thyroid: Higher radiation dose and longer time since diagnosis are linked to an increased risk of developing thyroid lumps. These growths may be benign (not cancerous) or malignant (cancer). It is more common in girls than boys. An enlarged thyroid (goiter) may be caused by lumps in the thyroid.
Symptoms of thyroid late effects depend on whether there is too little or too much thyroid hormone in the body.
These and other symptoms may be caused by thyroid late effects or by other problems:
Hypothyroidism (too little thyroid hormone)
- feeling tired or weak
- being more sensitive to cold
- pale, dry skin
- coarse and thinning hair
- brittle fingernails
- hoarse voice
- puffy face
- muscle and joint aches and stiffness
- constipation
- menstrual periods that are irregular or heavier than normal
- weight gain for no known reason
- depression or trouble with memory or being able to concentrate
Rarely, hypothyroidism does not cause any symptoms.
Hyperthyroidism (too much thyroid hormone)
- feeling nervous, anxious, or moody
- trouble sleeping
- feeling tired or weak
- having shaky hands
- having a fast heartbeat
- having red, warm skin that may be itchy
- having fine, soft hair that is falling out
- having frequent or loose bowel movements
- weight loss for no known reason
- being more sensitive to heat
The only way to know if these symptoms are caused by thyroid late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the thyroid.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood hormone studies use a blood sample to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of thyroid-stimulating hormone (TSH) or free thyroxine (T4).
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure can show the size of the thyroid and whether there are nodules (lumps) on the thyroid.
Talk to the doctor about whether tests and procedures are needed to check for signs of thyroid late effects. If tests are needed, find out how often they should be done.
Hypothalamus and pituitary gland
Neuroendocrine late effects may be caused after treatment for certain childhood cancers.
The neuroendocrine system is the nervous system and the endocrine system working together.
Treatment for these and other childhood cancers may cause neuroendocrine late effects:
- acute lymphoblastic leukemia (ALL)
- brain and spinal cord tumors
- head and neck cancers
- cancers treated with a stem cell transplant
Treatment that affects the hypothalamus or pituitary gland increases the risk of neuroendocrine system late effects.
Childhood cancer survivors have an increased risk for neuroendocrine late effects. These effects are caused by radiation therapy to treat cancer in the brain near the hypothalamus or used as total-body irradiation before a stem cell transplant. The hypothalamus controls the way hormones are made and released into the bloodstream by the pituitary gland. These effects are also caused by surgery in the area of the hypothalamus, pituitary gland, or optic pathways.
Late effects that affect the hypothalamus may cause certain health problems.
Childhood cancer survivors who have neuroendocrine late effects may have abnormal levels of hormones made in the pituitary gland and released into the blood. Neuroendocrine late effects and related health problems include:
- Growth hormone deficiency: Growth hormone helps promote growth and control metabolism. A low level of growth hormone is a common late effect of radiation to the brain in childhood cancer survivors. The higher the radiation dose and the longer the time since treatment, the greater the risk of this late effect. A low level of growth hormone may also occur in childhood ALL and stem cell transplant survivors who received radiation therapy to the brain and spinal cord and/or chemotherapy.
A low level of growth hormone in childhood results in adult height that is shorter than normal. If the child's bones have not fully developed, low growth hormone levels may be treated with growth hormone replacement therapy beginning one year after the end of treatment.
- Adrenocorticotropin deficiency (ACTH): Adrenocorticotropic hormone controls the making of glucocorticoids. A low level of adrenocorticotropic hormone is an uncommon late effect. It may occur in survivors:
- of childhood brain tumors, other tumors, or blood cancers
- with low growth hormone levels or central hypothyroidism
- who received radiation therapy to the brain
- who received steroid hormone therapy
Symptoms of adrenocorticotropin deficiency may not be severe and may not be noticed. Symptoms include:
- weight loss for no known reason
- not feeling hungry
- nausea
- vomiting
- abdominal pain
- low blood pressure
- feeling tired
- dizziness
- muscle or joint pains
- darkening of the skin
- pale skin
- low blood sugar
- craving salts
Low levels of adrenocorticotropin may be treated with hydrocortisone therapy.
- Hyperprolactinemia: Prolactin controls the making of breast milk and has many other effects in the body. A high level of the hormone prolactin may occur after a high dose of radiation to the brain or surgery that affects part of the pituitary gland. A high level of prolactin may cause:
- puberty at a later age than normal
- flow of breast milk in a woman who is not pregnant or breastfeeding
- less frequent or no menstrual periods or menstrual periods with a very light flow
- hot flashes
- inability to become pregnant
- inability to have an erection needed for sexual intercourse
- lower sex drive (in men and women)
- low bone mineral density (osteopenia)
Sometimes there are no signs and symptoms. Treatment is rarely needed.
- Thyroid-stimulating hormone (TSH) deficiency: Thyroid-stimulating hormone controls the making of thyroid hormones. A low level of thyroid hormone may occur very slowly over time after radiation therapy to the brain. Thyroid-stimulating hormone deficiency may also be called central hyphothyroidism.
Sometimes the symptoms of thyroid-stimulating hormone deficiency are not noticed. Low thyroid hormone levels may cause slow growth and delayed puberty, as well as other symptoms. Learn more about the symptoms of hypothyroidism.
A low level of thyroid hormone may be treated with thyroid hormone replacement therapy.
- Luteinizing hormone or follicle-stimulating hormone imbalance: Luteinizing hormone and follicle-stimulating hormone control reproduction. Abnormal levels of these hormones can cause different health problems. The type of problem depends on the radiation dose and whether hormone levels are higher or lower than normal.
Childhood cancer survivors who had brain tumors near the hypothalamus or pituitary gland, who were treated with lower doses of radiation to the brain, or who have hydrocephalus may develop central precocious puberty (a condition that causes puberty to start before age 8 in girls and 9 in boys). Central precocious puberty happens when the brain releases luteinizing and follicle-stimulating hormones too soon in the child's development. This condition may be treated with gonadotropin-releasing hormone (GnRH) agonist therapy to delay puberty and help the child's growth.
Childhood cancer survivors who were treated with higher doses of radiation to the brain may have low levels of luteinizing hormone or follicle-stimulating hormone. This condition may be treated with sex hormone replacement therapy. The dose will depend on the child's age and whether the child has reached puberty.
- Central diabetes insipidus: Central diabetes insipidus may be caused by the absence of or low amounts of all of the hormones made in the front part of the pituitary gland and released into the blood. It may occur in childhood cancer survivors treated with surgery in the area of the hypothalamus or pituitary gland. Symptoms of central diabetes insipidus may include:
- making large amounts of urine
- feeling very thirsty
- fatigue
Symptoms of central diabetes insipidus in infants may include:
- vomiting
- diarrhea
- irritability
- slowed growth and development
- weight loss for no known reason
Certain tests and procedures are used to diagnose health problems in the neuroendocrine system.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry study uses a blood sample to measure the amounts of certain substances, such as glucose, released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
- Blood hormone studies use a blood sample to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of follicle-stimulating hormone, luteinizing hormone, estradiol, testosterone, cortisol, or free thyroxine (T4).
- Lipid profile studies use a blood sample to measure the amounts of triglycerides, cholesterol, and low- and high-density lipoprotein cholesterol in the blood.
Talk to the doctor about whether tests and procedures are needed to check for signs of neuroendocrine late effects. If tests are needed, find out how often they should be done.
Metabolic syndrome
Metabolic syndrome is more likely to occur after treatment for certain childhood cancers.
Metabolic syndrome is a group of medical conditions that includes having too much fat around the abdomen and at least two of the following:
- high blood pressure
- high levels of triglycerides and low levels of high-density lipoprotein (HDL) cholesterol in the blood
- high levels of glucose (sugar) in the blood
Treatment for these and other childhood cancers may cause metabolic syndrome to occur later in life:
- acute lymphoblastic leukemia (ALL)
- cancers treated with a stem cell transplant
- cancers treated with radiation to the abdomen, such as Wilms tumor or neuroblastoma
Radiation therapy increases the risk of metabolic syndrome.
The risk of metabolic syndrome may be increased in childhood cancer survivors after treatment with:
- radiation therapy to the brain, abdomen, or pelvis
- total-body irradiation (TBI) as part of a stem cell transplant
- chemotherapy, such as alkylating agents
- older age
Certain tests and procedures are used to diagnose metabolic syndrome.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry studies use a blood sample to measure the amounts of certain substances, such as glucose, released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
- Lipid profile studies use a blood sample to measure the amounts of triglycerides, cholesterol, and low- and high-density lipoprotein cholesterol in the blood.
Talk to the doctor about whether tests and procedures are needed to check for signs of metabolic syndrome. If tests are needed, find out how often they should be done.
Metabolic syndrome may cause heart and blood vessel disease and diabetes.
Metabolic syndrome is linked to an increased risk of heart and blood vessel disease and diabetes. Health habits that decrease these risks include:
- having a healthy weight
- eating a heart-healthy diet
- exercising regularly
- not smoking
Weight changes and frailty
Weight changes and frailty are late effects that are more likely to occur after treatment for certain childhood cancers.
Weight changes include being underweight or having excess body weight or obesity. Frailty is a condition that usually affects older adults and includes having fatigue, slow walking speed, and muscle weakness.
Treatment for these and other childhood cancers may cause a change in weight or frailty:
- acute lymphoblastic leukemia (ALL)
- brain tumors, especially craniopharyngiomas
- bone tumors
- cancers treated with radiation to the brain, including TBI as part of a stem cell transplant
Graft-versus-host disease may also cause a change in weight for patients treated with a stem cell transplant.
Radiation therapy increases the risk of weight changes and frailty.
The risk of being underweight increases after treatment with:
- TBI for females
- radiation therapy to the abdomen for males
- certain types of chemotherapy (alkylating agents and anthracyclines)
The following may also increase the risk of being underweight:
- being female
- having a low household income
- having a chronic illness
The risk of having excess body weight or obesity increases after treatment with:
- radiation therapy to the brain
- surgery that damages the hypothalamus or pituitary gland, such as surgery to remove a craniopharyngioma brain tumor
The following may also increase the risk of obesity:
- having excess body weight at the time of a cancer diagnosis
- being diagnosed with cancer between the ages of 5 and 9
- being female
- having growth hormone deficiency or low levels of the hormone leptin
- lack of physical activity
- taking an antidepressant called paroxetine
Childhood cancer survivors who get enough exercise and have a normal amount of anxiety have a lower risk of obesity.
The risk of frailty increases after treatment with:
- radiation therapy to the brain
- TBI
Certain tests and procedures are used to diagnose a change in weight.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry studies use a blood sample to measure the amounts of certain substances, such as glucose, released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
- Lipid profile studies use a blood sample to measure the amounts of triglycerides, cholesterol, and low- and high-density lipoprotein cholesterol in the blood.
Being underweight, having excess body weight, or having obesity may be measured by weight, body mass index, percent of body fat, or size of the abdomen (belly fat).
Talk to the doctor about whether tests and procedures are needed to check for signs of a change in weight. If tests are needed, find out how often they should be done.
Immune System
Key Points
- Cancer treatments and surgery to remove the spleen increase the risk of immune system late effects.
- Late effects that affect the immune system may cause infection.
- Children who have had their spleen removed or have lost vaccine immunity may need antibiotics or booster vaccine doses to lessen the risk of infection.
Cancer treatments and surgery to remove the spleen increase the risk of immune system late effects.
The risk of health problems that affect the immune system increases after treatment that affects the spleen, including:
- surgery to remove the spleen
- high-dose radiation therapy to the spleen that causes the spleen to stop working
- stem cell transplant followed by graft-versus-host disease that causes the spleen to stop working
The risk of health problems that affect the immune system may increase after treatment with:
- chemotherapy
- radiation therapy
- stem cell transplant with or without graft-versus-host disease
Late effects that affect the immune system may cause infection.
Late effects that affect the immune system may increase the risk of viral infections or very serious bacterial infections. This risk is higher in younger children than in older children and in children who have decreased vaccine coverage after cancer treatment. The risk may be greater in the early years after the spleen stops working or is removed by surgery. These symptoms may be caused by infection:
- redness, swelling, or warmth of a part of the body
- pain that is in one part of the body, such as the eye, ear, or throat
- fever
An infection may cause other symptoms that depend on the part of the body affected. For example, a lung infection may cause a cough and trouble breathing.
Children who have had their spleen removed or have lost vaccine immunity may need antibiotics or booster vaccine doses to lessen the risk of infection.
Daily antibiotics may be prescribed for children younger than 5 years whose spleen is no longer working or for at least 1 year after surgery to remove the spleen. For certain high-risk patients, daily antibiotics may be prescribed throughout childhood and into adulthood.
In addition, children with an increased risk of infection should be vaccinated on a schedule through adolescence against:
- pneumococcal disease
- meningococcal disease
- Haemophilus influenzae type b (Hib) disease
- diphtheria-tetanus-pertussis (DTaP)
- hepatitis B
- measles
- mumps
Some children may lose the protection they had from vaccines during their cancer treatments. Talk to the doctor about whether childhood vaccinations given before cancer treatment need to be repeated.
Musculoskeletal System
Key Points
- Bone and joint late effects are more likely to occur after treatment for certain childhood cancers.
- Radiation therapy, surgery, chemotherapy, and other treatments increase the risk of bone and joint late effects.
- Radiation therapy
- Surgery
- Chemotherapy and other drug therapy
- Stem cell transplant
- Possible symptoms of bone and joint late effects include swelling over a bone or bone and joint pain.
- Certain tests and procedures are used to diagnose health problems in the bone and joint.
Bone and joint late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause bone and joint late effects:
- acute lymphoblastic leukemia (ALL)
- bone cancer
- brain and spinal cord tumors
- Ewing sarcoma
- head and neck cancers
- neuroblastoma
- non-Hodgkin lymphoma
- osteosarcoma
- retinoblastoma
- soft tissue sarcoma, such as rhabdomyosarcoma
- Wilms tumor
- cancers treated with a stem cell transplant
Poor nutrition and not enough exercise may also cause bone late effects.
Radiation therapy, surgery, chemotherapy, and other treatments increase the risk of bone and joint late effects.
Radiation therapy
Radiation therapy can stop or slow the growth of bone and muscle. The type of bone and joint late effects depends on the part of the body that received radiation therapy. Radiation therapy may cause:
- changes in the way the face or skull form, especially when high-dose radiation with or without chemotherapy is given to children before age 5 years
- short stature (being shorter than normal)
- curving of the spine (scoliosis) or rounding of the spine (kyphosis)
- one arm or leg is shorter than the other arm or leg
- weak or thin bones that can break easily (osteoporosis)
- parts of a bone to die from a lack of blood flow (osteoradionecrosis), especially the jaw
- a benign tumor of the bone (osteochondroma)
Surgery
Amputation or limb-sparing surgery to remove the cancer and prevent it from coming back may cause late effects depending on where the tumor was, age of the patient, and type of surgery. Health problems after amputation or limb-sparing surgery may include:
- having problems with activities of daily living
- not being able to be as active as normal
- chronic pain
- problems with the way prosthetics fit or work
- broken bone
- additional surgeries later in life
- the bone not healing well after surgery
- one arm or leg is shorter than the other
Studies show no difference in quality of life for childhood cancer survivors who had amputation compared to those who had limb-sparing surgery.
Chemotherapy and other drug therapy
Risk may be increased in childhood cancer survivors who received cancer treatment that included methotrexate or corticosteroids or glucocorticoids such as dexamethasone. Drug therapy may cause:
- weak or thin bones that can break easily (osteoporosis)
- one or more parts of a bone to die from a lack of blood flow (osteonecrosis), especially in the hip or knee
Stem cell transplant
A stem cell transplant can affect the bone and joints in different ways:
- Total-body irradiation given as part of a stem cell transplant may affect the body's ability to make growth hormone and cause short stature (being shorter than normal). It may also cause weak or thin bones that can break easily (osteoporosis) and the formation of a benign tumor called osteochondroma.
- Chronic graft-versus-host disease that may occur after a stem cell transplant can cause the muscles around joints to tighten, leading to stiff joints (joint contractures). Chronic graft-versus-host disease may also cause one or more parts of a bone to die from a lack of blood flow (osteonecrosis).
Possible symptoms of bone and joint late effects include swelling over a bone or bone and joint pain.
These and other symptoms may be caused by bone and joint late effects or by other problems:
- swelling over a bone or bony part of the body
- pain in a bone or joint
- redness or warmth over a bone or joint
- joint stiffness or trouble moving normally
- a bone that breaks easily or for no known reason
- short stature (being shorter than normal)
- one side of the body looks higher than the other side or the body tilts to one side
- always sitting or standing in a slouching position or having the appearance of a hunched back
The only way to know if these symptoms are caused by bone and joint late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the bone and joint.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Bone mineral density scan is an imaging test that measures bone density (the amount of bone mineral in a certain amount of bone) by passing x-rays with two different energy levels through the bone. It is used to diagnose osteoporosis (weak or thin bones that can break easily). Also called BMD scan, DEXA, DEXA scan, dual energy x-ray absorptiometric scan, dual x-ray absorptiometry, and DXA.
- X-ray is a type of radiation that can go through the body and make pictures of areas inside the body, such as bones.
- Vitamin D test uses a sample of blood to measure the amount of vitamin D in the body. Vitamin D is a nutrient the body needs to build and maintain strong bones.
- Calcium blood test uses a sample of blood to measure the amount of calcium in the body. Calcium is a mineral the body needs to build and maintain strong bones.
Talk to the doctor about whether tests and procedures are needed to check for signs of bone and joint late effects. If tests are needed, find out how often they should be done.
Reproductive System
Key Points
- Reproductive system late effects are more likely to occur after treatment for certain childhood cancers.
- Surgery, radiation therapy, and certain types of chemotherapy increase the risk of late effects that affect the reproductive system.
- Testicles
- Late effects that affect the testicles may cause certain health problems.
- Certain tests and procedures are used to diagnose health problems in the testicles.
- Ovaries
- Late effects that affect the ovaries may cause certain health problems.
- Possible symptoms of ovarian late effects include irregular or absent menstrual periods and hot flashes.
- Certain tests and procedures are used to diagnose health problems in the ovaries.
- Fertility and reproduction
- Childhood cancer survivors may have late effects that affect pregnancy.
- There are methods that may be used to help childhood cancer survivors have children.
- Children of childhood cancer survivors are not affected by the parent's previous treatment for cancer.
Reproductive system late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause testicular late effects:
- acute lymphoblastic leukemia (ALL)
- Ewing sarcoma
- germ cell tumors
- Hodgkin lymphoma
- non-Hodgkin lymphoma
- rhabdomyosarcoma
- soft tissue sarcoma
- testicular cancer
- cancers treated with a stem cell transplant
Treatment for these and other childhood cancers may cause ovarian late effects:
- acute lymphoblastic leukemia (ALL)
- germ cell tumors
- Hodgkin lymphoma
- Wilms tumor
- neuroblastoma
- cancers treated with a stem cell transplant
Surgery, radiation therapy, and certain types of chemotherapy increase the risk of late effects that affect the reproductive system.
The risk of health problems that affect the reproductive system increases after treatment with:
- surgery, such as the removal of a testicle, part of the prostate, lymph nodes in the abdomen, or one or both ovaries
- chemotherapy with alkylating agents, such as cyclophosphamide, dacarbazine, procarbazine, ifosfamide, mechlorethamine, cisplatin, lomustine, and busulfan
- radiation therapy to the abdomen, pelvis, lower back, testicles, ovaries, uterus, or in the area of the hypothalamus in the brain
- total-body irradiation, high-dose chemotherapy, or both before a stem cell transplant
- radiation therapy to the abdomen or pelvis with alkylating agents
In female survivors who had radiation therapy to the abdomen, the damage to the ovaries depends on the radiation dose, age at the time of treatment, and whether all or part of the abdomen received radiation.
Testicles
Late effects that affect the testicles may cause certain health problems.
Late effects of the testicles and related health problems include:
- Low sperm count: A zero sperm count or a low sperm count may be temporary or permanent. This depends on the radiation dose and schedule, the area of the body treated, and the age when treated.
- Low testosterone levels: This can lead to underdeveloped testicles, infertility, and sexual problems in adulthood.
- Infertility: The inability to father a child.
- Retrograde ejaculation: Very little or no semen comes out of the penis during orgasm.
After treatment with chemotherapy or radiation, the body's ability to make sperm may come back over time.
Certain tests and procedures are used to diagnose health problems in the testicles.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests:
- Blood hormone studies use a blood sample to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of follicle-stimulating hormone, luteinizing hormone, testosterone.
- Semen analysis (sperm count) measures the amount and quality of semen and sperm to see if there are problems that are causing infertility.
Ovaries
Late effects that affect the ovaries may cause certain health problems.
Ovarian late effects and other health-related problems include:
- early menopause, especially in women who had their ovaries removed or were treated with both an alkylating agent and radiation therapy to the abdomen
- changes in menstrual periods
- infertility (inability to conceive a child)
- puberty does not begin
Hormone replacement therapy can be used to start puberty.
Possible symptoms of ovarian late effects include irregular or absent menstrual periods and hot flashes.
These and other symptoms may be caused by ovarian late effects or by other problems:
- irregular or no menstrual periods
- hot flashes
- drenching night sweats
- trouble sleeping
- mood changes
- lowered sex drive
- vaginal dryness
- sex traits, such as developing arm, pubic, and leg hair or having the breasts enlarge, do not occur at puberty
- weak or thin bones that can break easily (osteoporosis)
- inability to get pregnant
The only way to know if these symptoms are caused by late effects to the ovaries is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the ovaries.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following test.
- Blood hormone studies use a blood sample to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of follicle-stimulating hormone, luteinizing hormone, estradiol, or TSH.
Fertility and reproduction
Childhood cancer survivors may have late effects that affect pregnancy.
Late effects on pregnancy include increased risk of:
- high blood pressure
- diabetes during pregnancy
- anemia
- miscarriage or stillbirth
- low birth-weight babies
- early labor and/or delivery
- impaired blood flow to the uterus
- delivery by Cesarean section
- the fetus is not in the right position for birth (for example, the foot or buttock is in position to come out before the head)
- peripartum cardiomyopathy
Long-term survivors of childhood, adolescent, and young adult cancers who have received radiation therapy or certain types of chemotherapy are at risk of a rare type of heart failure during pregnancy called peripartum cardiomyopathy. It may occur during late pregnancy and up to 5 months after giving birth. If cancer treatments have caused damage to the heart, these patients may also be at risk of congestive heart failure during pregnancy. Patients at risk of these conditions should be closely followed for weakness of the heart muscle during pregnancy.
Some studies have not shown an increased risk of late effects on pregnancy.
There are methods that may be used to help childhood cancer survivors have children.
The following methods may be used so that childhood cancer survivors can have children:
- freezing the eggs or sperm before cancer treatment in patients who have reached puberty (egg and sperm banking)
- preventing damage to the ovaries before radiation therapy by moving one or both ovaries and fallopian tubes out of the field of radiation and attaching them to the wall of the abdomen (ovarian transposition)
- removing a small amount of tissue containing sperm from the testicle (testicular sperm extraction)
- fertilizing an egg outside the body by injecting a sperm into it (intracytoplasmic sperm injection)
- in vitro fertilization (IVF), which is a procedure where eggs and sperm are placed together in a container, giving the sperm the chance to enter an egg
Children of childhood cancer survivors are not affected by the parent's previous treatment for cancer.
The children of childhood cancer survivors do not appear to have an increased risk of birth defects, genetic disease, or cancer.
Respiratory System
Key Points
- Lung late effects are more likely to occur after treatment for certain childhood cancers.
- Certain types of chemotherapy and radiation to the lungs increase the risk of lung late effects.
- Late effects that affect the lungs may cause certain health problems.
- Possible symptoms of lung late effects include trouble breathing and cough.
- Certain tests and procedures are used to diagnose health problems in the lung.
- Health habits that promote healthy lungs are important for survivors of childhood cancer.
Lung late effects are more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause lung late effects:
- germ cell tumors
- head and neck cancers
- Hodgkin lymphoma
- leukemia
- neuroblastoma
- Wilms tumor
- cancers treated with a stem cell transplant
Certain types of chemotherapy and radiation to the lungs increase the risk of lung late effects.
The risk of health problems that affect the lungs increases after treatment with:
- surgery to remove all or part of the lung or chest wall
- chemotherapy, such as bleomycin, busulfan, carmustine, or lomustine
- total-body irradiation or high-dose chemotherapy before a stem cell transplant
- radiation therapy to the chest
In survivors who had radiation to the chest, the damage to the lungs and chest wall depends on the radiation dose, whether all or part of the lungs and chest wall received radiation, whether the radiation was given in small, divided daily doses, and the child's age at treatment.
The risk of lung late effects is greater in childhood cancer survivors who are treated with a combination of surgery, chemotherapy, and/or radiation therapy. The risk is also increased in survivors who have a history of:
- infections or graft-versus-host disease after a stem cell transplant
- lung or airway disease, such as asthma, before cancer treatment
- an abnormal chest wall
- smoking cigarettes or other substances
Late effects that affect the lungs may cause certain health problems.
Lung late effects and related health problems include:
- inflamed lung caused by radiation therapy (radiation pneumonitis)
- buildup of scar tissue in the lung (pulmonary fibrosis)
- other lung and airway problems, such as chronic obstructive pulmonary disease (COPD), pneumonia, pneumothorax, cough that does not go away, and asthma
Possible symptoms of lung late effects include trouble breathing and cough.
These and other symptoms may be caused by lung late effects or by other problems:
- shortness of breath (dyspnea), especially when being active
- wheezing
- fever
- chronic cough
- congestion (a feeling of fullness in the lungs from extra mucus)
- chronic lung infections
- feeling tired
The only way to know if these symptoms are caused by lung late effects is to see a doctor.
Lung late effects in childhood cancer survivors may occur slowly over time or there may be no symptoms. Sometimes lung damage can be detected only by imaging or pulmonary function testing. Lung late effects may improve over time.
Certain tests and procedures are used to diagnose health problems in the lung.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Chest x-ray is an x-ray of the organs and bones inside the chest. An x-ray is a type of radiation that can go through the body and make pictures of areas inside the body.
- Pulmonary function test (PFT) is a test to see how well the lungs are working. It measures how much air the lungs can hold and how quickly air moves into and out of the lungs. It also measures how much oxygen is used and how much carbon dioxide is given off during breathing. This is also called lung function test.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the chest. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
Talk to the doctor about whether tests and procedures are needed to check for signs of lung late effects. If tests are needed, find out how often they should be done.
Health habits that promote healthy lungs are important for survivors of childhood cancer.
Childhood cancer survivors with lung late effects should take care to protect their health, including:
- Not smoking. Self-help programs and counseling are available to those who want to quit. Learn more about the health risks of cigarette smoking and how to quit.
- Getting vaccines for flu and pneumococcus.
Senses
Key Points
- Hearing
- Hearing problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
- Radiation therapy to the brain and certain types of chemotherapy increase the risk of hearing loss.
- Hearing loss is the most common sign of hearing late effects.
- Certain tests and procedures are used to diagnose health problems in the ear and hearing problems.
- Seeing
- Eye and vision problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
- Radiation therapy to the brain or head increases the risk of eye problems or vision loss.
- Late effects that affect the eye may cause certain health problems.
- Possible signs and symptoms of eye and vision late effects include changes in vision and dry eyes.
- Certain tests and procedures are used to diagnose health problems in the eye and vision problems.
Hearing
Hearing problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause hearing late effects:
- bone cancer
- brain tumors
- germ cell tumors
- head and neck cancers
- liver cancer
- neuroblastoma
- retinoblastoma
- soft tissue sarcoma
- cancers that are treated with a stem cell transplant
Radiation therapy to the brain and certain types of chemotherapy increase the risk of hearing loss.
The risk of hearing loss is increased in childhood cancer survivors after treatment with:
- certain types of chemotherapy, such as cisplatin or high-dose carboplatin
- radiation therapy to the brain
The risk of hearing loss from radiation therapy is greater in children who are diagnosed with cancer before age 5 years, and the risk increases for children of all ages with higher radiation doses. The risk of hearing loss is also greater in childhood cancer survivors who received radiation therapy to the brain and chemotherapy at the same time.
The risk of hearing loss may be lower if children treated with cisplatin were also given a drug called sodium thiosulfate.
Hearing loss is the most common sign of hearing late effects.
These and other symptoms may be caused by hearing late effects or by other problems:
- hearing loss
- ringing in the ears
- feeling dizzy
- too much hardened wax in the ear
The only way to know if these symptoms are caused by hearing late effects is to see a doctor.
Hearing loss may occur during treatment, soon after treatment ends, or several months or years after treatment ends and worsen over time. A young child may have trouble learning, communicating, doing well in school, and interacting with others if they have hearing loss. In adulthood, hearing loss can lead to social isolation, depression, anxiety, and trouble finding stable employment. Talk to a doctor to learn about hearing aids or other ways to cope with hearing loss.
Certain tests and procedures are used to diagnose health problems in the ear and hearing problems.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Otoscopic exam is an exam of the ear. An otoscope is used to look at the ear canal and the eardrum to check for signs of infection or hearing loss. Sometimes the otoscope has a plastic bulb that is squeezed to release a small puff of air into the ear canal. In a healthy ear, the eardrum will move. If there is fluid behind the eardrum, it will not move.
- Hearing test can be done in different ways depending on a person's age. The test is done to check if the person can hear soft and loud sounds and low- and high-pitched sounds. Each ear is checked separately.
Talk to the doctor about whether tests and procedures are needed to check for signs of hearing late effects. If tests are needed, find out how often they should be done.
Seeing
Eye and vision problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause eye and vision late effects:
- acute lymphoblastic leukemia (ALL)
- brain tumors
- head and neck cancers
- retinoblastoma, rhabdomyosarcoma, and other tumors of the eye
- cancers treated with total-body irradiation (TBI) before a stem cell transplant
Radiation therapy to the brain or head increases the risk of eye problems or vision loss.
The risk of eye problems or vision loss may be increased in childhood cancer survivors after treatment with:
- radiation therapy to the brain, eye, or eye socket
- surgery to remove the eye or a tumor near the optic nerve
- certain types of chemotherapy, such as cytarabine and doxorubicin
- TBI, busulfan, and corticosteroids as part of a stem cell transplant
Having a history of chronic graft-versus-host disease after a stem cell transplant can also increase the risk of eye problems and vision loss.
Late effects that affect the eye may cause certain health problems.
Eye late effects and related health problems include:
Possible signs and symptoms of eye and vision late effects include changes in vision and dry eyes.
These and other symptoms may be caused by eye and vision late effects or by other problems:
- changes in vision, such as:
- not being able to see objects that are close
- not being able to see objects that are far away
- double vision
- cloudy or blurred vision
- colors seem faded
- being sensitive to light or trouble seeing at night
- seeing a glare or halo around lights at night
- dry eyes that may feel like they are itchy, burning, or swollen, or like there is something in the eye
- eye pain
- eye redness
- having a growth on the eyelid
- drooping of the upper eyelid
The only way to know if these symptoms are caused by eye and vision late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the eye and vision problems.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Eye exam with dilated pupil is when the pupil is dilated (widened) with medicated eye drops to allow the doctor to look through the lens and pupil to the retina. The inside of the eye, including the retina and the optic nerve, is checked using an instrument that makes a narrow beam of light. This is sometimes called a slit-lamp exam. If there is a tumor, the doctor may take pictures over time to keep track of changes in the size of the tumor and how fast it is growing.
- Indirect ophthalmoscopy is an exam of the inside of the back of the eye using a small magnifying lens and a light.
Talk to the doctor about whether tests and procedures are needed to check for signs of eye and vision late effects. If tests are needed, find out how often they should be done.
Urinary System
Key Points
- Kidney
- Kidney problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
- Certain types of chemotherapy increase the risk of kidney late effects.
- Late effects that affect the kidney may cause certain health problems.
- Possible symptoms of kidney late effects include problems urinating and swelling of the feet or hands.
- Certain tests and procedures are used to diagnose health problems in the kidney.
- Health habits that promote healthy kidneys are important for survivors of childhood cancer.
- Bladder
- Bladder problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
- Surgery to the pelvic area and certain types of chemotherapy increase the risk of bladder late effects.
- Late effects that affect the bladder may cause certain health problems.
- Possible symptoms of bladder late effects include changes in urination and swelling of the feet or hands.
- Certain tests and procedures are used to diagnose health problems in the bladder.
Kidney
Kidney problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause kidney late effects:
- Wilms tumor
- cancers treated with a stem cell transplant
Certain types of chemotherapy increase the risk of kidney late effects.
The risk of health problems that affect the kidney increases after treatment with:
- chemotherapy including cisplatin, carboplatin, ifosfamide, and methotrexate
- radiation therapy to the abdomen or middle of the back
- surgery to remove part or all of a kidney
- stem cell transplant
The risk of kidney late effects is greater in childhood cancer survivors who were treated with a combination of surgery, chemotherapy, or radiation therapy.
The following may also increase the risk of kidney late effects:
- having cancer in both kidneys
- having a genetic syndrome that increases the risk of kidney problems, such as Denys-Drash syndrome or WAGR syndrome
- being treated with more than one type of treatment
Late effects that affect the kidney may cause certain health problems.
Kidney late effects or related health problems include:
- damage to the parts of the kidney that filter and clean the blood or the parts that remove extra water from the blood
- loss of electrolytes, such as magnesium, calcium, or potassium, from the body
- high blood pressure (hypertension)
Possible symptoms of kidney late effects include problems urinating and swelling of the feet or hands.
These and other symptoms may be caused by kidney late effects or by other problems:
- feeling the need to urinate without being able to do so
- frequent urination (especially at night)
- trouble urinating
- feeling very tired
- swelling of the legs, ankles, feet, face, or hands
- itchy skin
- shortness of breath
- nausea or vomiting
- loss of appetite
- a metal-like taste in the mouth or bad breath
- headache
Sometimes there are no signs or symptoms in the early stages. Signs or symptoms may appear as damage to the kidney continues over time. The only way to know if these symptoms are caused by kidney late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the kidney.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry study uses a blood sample to measure the amounts of certain substances, such as creatinine, released into the blood by organs and tissues in the body. An unusual amount of a substance may be a sign of kidney disease.
- Urinalysis checks the color of urine and its contents, such as sugar, protein, red blood cells, and white blood cells.
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs, such as the kidney, and make echoes. The echoes form a picture of body tissues called a sonogram.
Talk to the doctor about whether tests and procedures are needed to check for signs of kidney late effects. If tests are needed, find out how often they should be done.
If kidney problems are found, treatment options are available, including kidney transplant.
Health habits that promote healthy kidneys are important for survivors of childhood cancer.
Childhood cancer survivors who had all or part of their kidney removed should talk to their doctor about:
- whether it is safe to play sports that have a high risk of heavy contact or impact such as football or hockey
- bicycle safety and avoiding handlebar injuries
- wearing a seatbelt around the hips, not the waist
Bladder
Bladder problems are a late effect that is more likely to occur after treatment for certain childhood cancers.
Treatment for these and other childhood cancers may cause bladder late effects:
- retinoblastoma
- cancers treated with a stem cell transplant
Surgery to the pelvic area and certain types of chemotherapy increase the risk of bladder late effects.
The risk of health problems that affect the bladder increases after treatment with:
- surgery to remove part or all of the bladder
- surgery to the pelvis, spine, or brain
- certain types of chemotherapy, such as cyclophosphamide or ifosfamide
- radiation therapy to areas near the bladder, pelvis, or urinary tract
- stem cell transplant
Late effects that affect the bladder may cause certain health problems.
Bladder late effects and related health problems include:
- inflammation of the inside of the bladder wall, which leads to bleeding (hemorrhagic cystitis)
- thickening of the bladder wall
- decreased urine storage
- trouble emptying the bladder
- incontinence
- a blockage in the kidney, ureter, bladder, or urethra
- urinary tract infections that last a long time or keep coming back
Possible symptoms of bladder late effects include changes in urination and swelling of the feet or hands.
These and other symptoms may be caused by bladder late effects or by other problems:
- feeling the need to urinate without being able to do so
- frequent urination (especially at night)
- trouble urinating
- feeling like the bladder does not empty completely after urination
- swelling of the legs, ankles, feet, face, or hands
- little or no bladder control
- blood in the urine
The only way to know if these symptoms are caused by bladder late effects is to see a doctor.
Certain tests and procedures are used to diagnose health problems in the bladder.
In addition to asking the childhood cancer survivor about their personal and family health history and doing a physical exam, the doctor may perform the following tests and procedures:
- Blood chemistry study uses a blood sample to measure the amounts of certain substances, such as magnesium, calcium, and potassium, released into the blood by organs and tissues in the body. An unusual amount of a substance may be a sign of bladder problems.
- Urinalysis checks the color of urine and its contents, such as sugar, protein, red blood cells, and white blood cells.
- Urine culture checks for bacteria, yeast, or other microorganisms in the urine when there are symptoms of infection. Urine cultures can help identify the type of microorganism that is causing an infection. Treatment of the infection depends on the type of microorganism that is causing the infection.
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs, such as the bladder, and make echoes. The echoes form a picture of body tissues called a sonogram.
Talk to the doctor about whether tests and procedures are needed to check for signs of bladder late effects. If tests are needed, find out how often they should be done.
To Learn More About Late Effects of Treatment for Childhood Cancer
For more information about late effects of treatment for childhood cancer:
- Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers
- Late Effects Directory of Services
- Computed Tomography (CT) Scans and Cancer
For more childhood cancer information and other general cancer resources from the National Cancer Institute:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the late effects of treatment for childhood cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Late Effects of Treatment for Childhood Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/childhood-cancers/late-effects-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389365]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Updated:
Source URL: https://www.cancer.gov/node/5770/syndication
Source Agency: National Cancer Institute (NCI)
Captured Date: 2013-09-14 09:03:05.0