Craniopharyngioma Treatment
If your child has been diagnosed with a craniopharyngioma—a rare, noncancerous tumor that develops in the brain near the pituitary gland and hypothalamus—you want caring, experienced doctors at their side. You’ll find them at Montefiore Einstein Comprehensive Cancer Center at the Children’s Hospital at Montefiore Einstein (CHAM).
Our team includes internationally recognized physicians who specialize in childhood brain tumors. They offer the most up-to-date treatments and innovative clinical trials based on discoveries from the ongoing research that happens at Montefiore Einstein Comprehensive Cancer Center. You’ll also find compassionate and highly skilled nurses, specialists and support staff, collaborating to ensure your child will receive the best care in a supportive and nurturing environment.
When you need care for your child, you can feel confident turning to Montefiore Einstein Comprehensive Cancer Center at CHAM, where we address your child’s whole health needs.

Cancer Clinical Trials
- Blood & Bone Marrow Cancers
- Brain, Spine & Central Nervous System Cancers
- Breast Cancer
- Childhood Cancers
- Endocrine System Cancers
- Gastrointestinal (GI) Cancers
- Genitourinary (GU) & Urologic Cancers
- Gynecologic Cancers
- Head & Neck Cancers
- Kaposi Sarcoma & AIDS-Related Cancers
- Lung & Chest Cancers
- Prostate Cancer
- Sarcomas
- Skin Cancer
As an NCI-designated comprehensive cancer center, Montefiore Einstein Comprehensive Cancer Center supports the mission and guidelines of the National Cancer Institute (NCI). The following information about types of cancer, prevention and treatments is provided by the NCI.
Childhood Craniopharyngioma (PDQ®)–Patient Version
What is childhood craniopharyngioma?
Childhood craniopharyngioma is a rare tumor usually found near the pituitary gland (a pea-sized organ at the bottom of the brain that controls other glands) and the hypothalamus (a small cone-shaped organ connected to the pituitary gland by nerves). Craniopharyngiomas can occur at any age but are most often diagnosed in children aged 5 to 14 years and older adults. They are rare in children younger than 2.
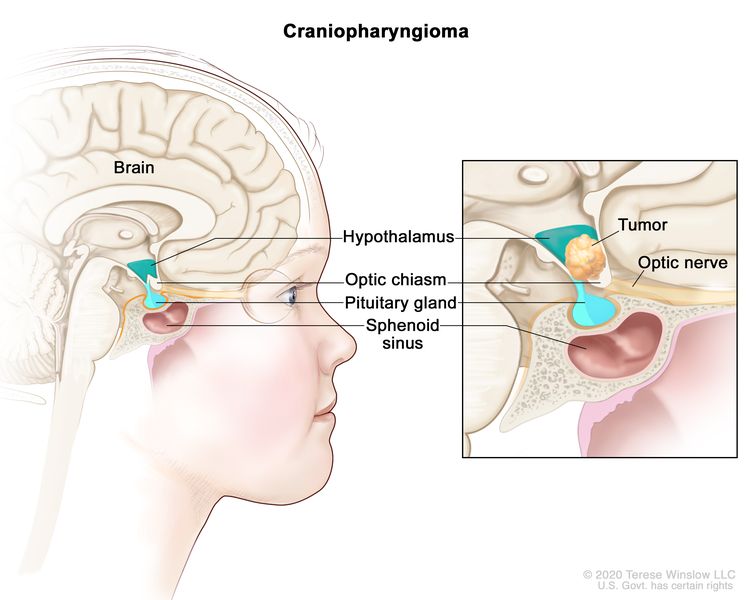
Craniopharyngiomas are rare brain tumors that usually form near the pituitary gland and the hypothalamus. They are benign (not cancer) and do not spread to other parts of the brain or to other parts of the body. However, they may grow and press on nearby parts of the brain, including the pituitary gland, optic chiasm, and optic nerve. Craniopharyngiomas usually occur in children and young adults.
Craniopharyngiomas are usually part solid mass and part fluid-filled cyst. They are not cancer and do not spread to other parts of the brain or other parts of the body. However, they can grow and press on nearby parts of the brain, such as the pituitary gland. Or they may press on other areas, such as:
- the optic chiasm
- the optic nerves
- the fluid-filled spaces in the brain
Craniopharyngiomas may affect many brain functions, including hormone production, growth, and vision. Treatments help stop the tumor from pushing on other areas of the brain.
Causes and risk factors for childhood craniopharyngioma
Craniopharyngioma is caused by certain changes to the way the brain cells function, especially how they grow and divide into new cells. Often, the exact cause of these changes is unknown.
There are no known risk factors for childhood craniopharyngioma.
Symptoms of childhood craniopharyngioma
The symptoms of childhood craniopharyngioma depend on where the tumor grows in the brain. It's important to check with your child's doctor if your child has:
- headaches, including morning headache or headache that goes away after vomiting
- vision changes
- nausea and vomiting
- loss of balance or trouble walking
- unusual sleepiness or change in energy level
- changes in personality or behavior
- an increase in thirst or urination
- a short stature or slow growth
- weight gain
- hearing loss
- early or late puberty
These symptoms may be caused by problems other than craniopharyngioma. The only way to know is for your child to see a doctor.
Some symptoms caused by the tumor may continue for months or years after treatment. It is important to talk with your child's doctors about problems that may continue after treatment.
Tests to diagnose childhood craniopharyngioma
In This Section
- Visual field exam
- CT scan (CAT scan)
- Magnetic resonance imaging (MRI) with gadolinium
- Blood hormone studies
- Biopsy
- Immunohistochemistry
If your child has symptoms that suggest a craniopharyngioma, the doctor will need to find out if they are due to a tumor or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will also ask about your child's personal and family medical history and do a physical exam, including a neurologic exam. Depending on these results, they may recommend other tests. If your child is diagnosed with craniopharyngioma, the results of these tests will help you and your child's doctor plan treatment.
The tests to diagnose craniopharyngioma may include:
Visual field exam
A visual field exam checks a person’s field of vision (the total area in which objects can be seen). This test measures both central vision (how much a person can see when looking straight ahead) and peripheral vision (how much a person can see in all other directions while staring straight ahead). Any loss of vision may be a sign of a tumor that has damaged or pressed on the parts of the brain that affect eyesight.
CT scan (CAT scan)
CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
Magnetic resonance imaging (MRI) with gadolinium
MRI uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the brain and the spine. A substance called gadolinium is injected into a vein. The gadolinium collects around the tumor cells so they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Blood hormone studies
Blood hormone studies use a blood sample to measure the amounts of certain hormones released into the blood by organs and tissues in the body. If the amount of a hormone is higher or lower than normal, it can be a sign of disease in the organ or tissue that makes it. For craniopharyngioma, the blood may be checked for unusual levels of thyroid-stimulating hormone (TSH) or adrenocorticotropic hormone (ACTH). These hormones are made by the pituitary gland.
Biopsy
If the CT scan or MRI show there may be a brain tumor, your child will have a biopsy to remove a sample of the tumor.
Types of biopsy that may be used to take the sample of tissue include:
- Open biopsy: A surgeon inserts a hollow needle through a hole in the skull into the brain.
- Computer-guided needle biopsy: A surgeon inserts a hollow needle guided by a computer through a small hole in the skull into the brain.
- Transsphenoidal biopsy: The surgeon inserts instruments through the nose and sphenoid bone (a butterfly-shaped bone at the base of the skull) and into the brain.
A pathologist views the tissue under a microscope to look for tumor cells. If they find tumor cells, the surgeon will remove as much tumor as safely possible during the same surgery.
Immunohistochemistry
Immunohistochemistry uses antibodies to check for certain antigens (markers) in a sample of a patient’s cells or tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
Getting a second opinion
You may want to get a second opinion to confirm your child's diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. This doctor may agree with the first doctor, suggest changes to the treatment plan, or provide more information about your child's tumor.
To learn more about choosing a doctor and getting a second opinion, visit Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your child's appointments, visit Questions to Ask Your Doctor about Cancer.
Types of treatment for childhood craniopharyngioma
In This Section
- Who treats children with craniopharyngioma?
- Surgery
- Surgery for cysts
- Radiation therapy
- Chemotherapy
- Observation
- Clinical trials
- Treatment of newly diagnosed childhood craniopharyngioma
- Treatment of progressive or recurrent childhood craniopharyngioma
Who treats children with craniopharyngioma?
A pediatric oncologist, a doctor who specializes in treating children with cancer, oversees treatment for childhood craniopharyngioma. The pediatric oncologist works with other health care providers who are experts in treating children with brain tumors and who specialize in certain areas of medicine. Other specialists may include:
There are different types of treatment for children and adolescents with craniopharyngioma. Although craniopharyngioma is not cancer, treatment is often similar to cancer treatment and may include surgery, radiation therapy, and other approaches. You and your child's care team will work together to decide treatment. Many factors will be considered, such as your child's age and overall health, where the tumor is located and whether it has spread into nearby tissue, and the possible side effects and late effects of treatment.
Your child's treatment plan will include information about the tumor, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child's care team before treatment begins about what to expect. For help every step of the way, visit our booklet, Children with Cancer: A Guide for Parents.
Types of treatment your child might have include:
Surgery
The type of surgery your child will have depends on the size of the tumor, where it is in the brain, and whether it has grown into nearby tissue in a finger-like way. It also depends on expected late effects that may occur after surgery.
The types of surgery that may be used to remove the tumor that can be seen with the eye include:
- Transsphenoidal surgery is a type of surgery in which a surgeon inserts instruments into the brain by going through a cut made under the upper lip or at the bottom of the nose between the nostrils. Then they go through the sphenoid bone (a butterfly-shaped bone at the base of the skull) to reach the tumor near the pituitary gland and hypothalamus.
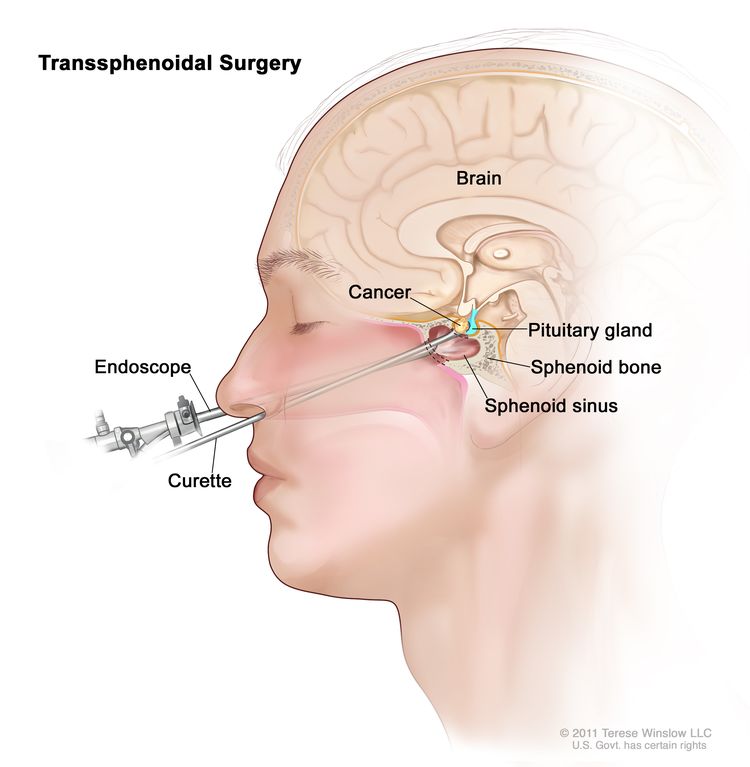
Transsphenoidal surgery. An endoscope and a curette are inserted through the nose and sphenoid sinus to remove the tumor.
- A craniotomy is surgery to remove the tumor through an opening made in the skull.
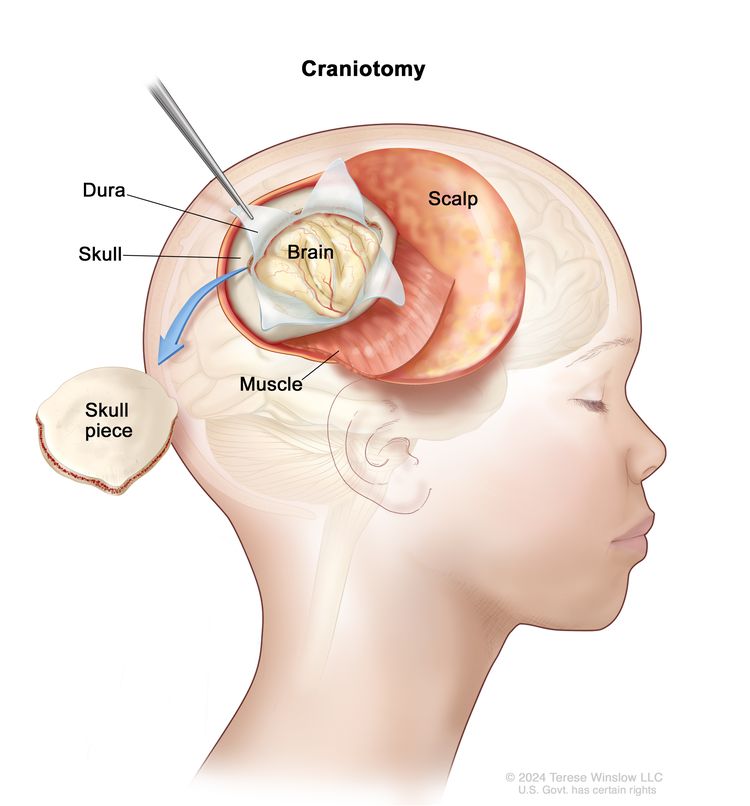
Craniotomy. An opening is made in the skull and a piece of the skull is removed to show part of the brain.
To help make a diagnosis, sometimes the surgeon will remove only part of the tumor. If a tumor is near the pituitary gland or hypothalamus, it will not be removed. Leaving the tumor helps reduce serious side effects from the surgery.
Sometimes, the surgeon will remove all of the tumor that they can see and no further treatment is needed. At other times, they may not be able to remove the tumor because it is growing into or pressing on nearby organs.
Surgery for cysts
If your child's tumor is mostly a fluid-filled cyst, they may have surgery to drain it. Draining it lowers the pressure in the brain and relieves symptoms.
A surgery called a partial resection can be used to remove fluid from cystic craniopharyngiomas. Or a thin tube called a catheter can be inserted into the cyst, and a small container placed under the skin. The fluid drains into the container and is later removed.
Sometimes, after the cyst is drained, a drug is put through the catheter into the cyst. This causes the inside wall of the cyst to scar and stops the cyst from making fluid. Or it can slow down how long it takes for the fluid to build up again. Surgery to remove the tumor or radiation therapy may be done after the cyst is drained.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill tumor cells or keep them from growing. It is often given after surgery to kill any tumor that is left in the brain.
Both external radiation therapy and internal radiation therapy (also called brachytherapy) are used to treat craniopharyngiomas.
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with the tumor.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the tumor.
Radiation therapy to the brain can affect growth and development in young children, so ways of giving radiation therapy that have fewer side effects are often used. These include:
- Stereotactic radiosurgery may be used for very small craniopharyngiomas at the base of the brain. For this treatment, a rigid head frame is attached to the skull to keep the head still during the treatment. Then, a machine aims a single large dose of radiation directly at the tumor. This procedure is a type of radiation therapy and does not involve surgery. It is also called stereotaxic radiosurgery, radiosurgery, and radiation surgery.
- Intracavitary radiation therapy is a type of internal radiation therapy that may be used in tumors that are part solid mass and part fluid-filled cyst. For this treatment, radioactive material is placed inside the tumor. This type of radiation therapy causes less damage to the nearby hypothalamus and optic nerves.
- Intensity-modulated photon therapy is a type of radiation therapy that uses x-rays or gamma rays that come from a special machine called a linear accelerator (linac) to kill tumor cells. A computer is used to target the exact shape and location of the tumor. Then thin beams of photons of different strengths are aimed at the tumor from many angles. This type of 3-dimensional radiation therapy may cause less damage to healthy tissue in the brain and other parts of the body.
- Proton-beam radiation therapy is a type of radiation therapy that uses streams of protons (tiny particles with a positive charge) to kill tumor cells. This treatment can reduce the amount of radiation damage to healthy tissue near a tumor.
Learn more about Radiation Therapy to Treat Cancer.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of tumor cells. Chemotherapy either kills the tumor cells or stops them from dividing.
Chemotherapy can be placed directly into a cavity, such as a cyst. This way of giving chemotherapy is intracavitary chemotherapy. Bleomycin is a type of chemotherapy that can be placed directly into a cystic craniopharyngioma.
Learn more about Chemotherapy to Treat Cancer.
Observation
Observation means that your child's condition is closely watched without receiving treatment until symptoms appear or change.
Clinical trials
For some children, joining a clinical trial may be an option. There are different types of clinical trials for childhood cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your child's age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment of newly diagnosed childhood craniopharyngioma
Treatment of newly diagnosed childhood craniopharyngioma may include:
- complete removal of the tumor with surgery with or without radiation therapy
- partial removal of the tumor with surgery followed by radiation therapy
- cyst drainage, followed by observation, radiation therapy, or surgery
- brachytherapy or chemotherapy placed directly in the cyst or tumor
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of progressive or recurrent childhood craniopharyngioma
Treatment options for progressive or recurrent childhood craniopharyngioma depend on the type of treatment that your child received when the tumor was first diagnosed and your child's needs.
Treatment may include:
- surgery
- external-beam radiation therapy
- brachytherapy or intracavitary chemotherapy
- observation
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Prognostic factors for childhood craniopharyngioma
If your child has been diagnosed with craniopharyngioma, you likely have questions about how serious the tumor is and your child's chances of survival. The likely outcome or course of a disease is called prognosis.
The prognosis depends on:
- the size of the tumor
- where the tumor is in the brain
- whether there are tumor cells left after surgery
- your child's age
- side effects that may occur months or years after treatment
- whether the tumor has just been diagnosed or has recurred (come back)
No two people are alike, and responses to treatment can vary greatly. While the prognosis for childhood craniopharyngioma is generally good, the tumor often comes back after surgery. Your child's treatment team is in the best position to talk with you about your child's prognosis.
Side effects and late effects of treatment
Cancer treatments used for craniopharyngioma can cause side effects. Which side effects your child might have depends on the type of treatment they receive, the dose, and how their body reacts. Talk with your child's treatment team about which side effects to look for and ways to manage them.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Problems from treatment that begin 6 months or later after treatment and continue for months or years are called late effects. Late effects of treatment may include:
- seizures
- bone and muscle growth and development
- behavior problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Serious physical problems may occur if the pituitary gland, hypothalamus, optic nerves, or carotid artery are affected during surgery or radiation therapy. These problems include:
- obesity
- metabolic syndrome, including fatty liver disease not caused by drinking alcohol
- vision problems, including blindness
- blood vessel problems or stroke
- loss of the ability to make certain hormones
Some late effects may be treated or controlled. Your child may need life-long hormone replacement therapy with several medicines. It is important to talk with your child's doctors about the effects treatment can have on your child. Learn more about Late Effects of Treatment for Childhood Cancer.
Follow-up care
Some of the tests that were done to diagnose the disease or decide how to treat it may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed. These tests are sometimes called follow-up tests or check-ups.
After treatment, follow-up testing with MRI will be done for several years to check if the tumor has come back.
Coping with your child's diagnosis
When your child has a tumor, every member of the family needs support. Taking care of yourself during this difficult time is important. Reach out to your child’s treatment team and to people in your family and community for support. To learn more, visit Support for Families When a Child Has Cancer and the booklet Children with Cancer: A Guide for Parents.
Related resources
For more childhood cancer information and other general cancer resources, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood craniopharyngioma. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Craniopharyngioma. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/brain/patient/child-cranio-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389237]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Updated:
Source URL: https://www.cancer.gov/node/6377/syndication
Source Agency: National Cancer Institute (NCI)
Captured Date: 2013-09-14 09:03:29.0