Our Approach to Pelvic Pain


The Montefiore Einstein Pelvic Pain Program is an internationally recognized leader, providing comprehensive, personalized care for women with the full range of pelvic pain conditions. Our multidisciplinary team of world-renowned gynecologists collaborates closely with experts in urology, urogynecology and pelvic reconstructive surgery, reproductive endocrinology and infertility, gastroenterology, pain management, physical therapy, interventional radiology, behavioral health and other disciplines to deliver compassionate, coordinated care that addresses the complex, multifactorial nature of pelvic pain. Utilizing the latest diagnostics and leading-edge therapies, we employ an evidence-based, individualized approach tailored to each patient’s unique needs and goals—recognizing that no two patients experience pelvic pain the same way. We are an international referral site for the most complex pelvic pain cases, providing second opinions, advanced diagnostics and specialized nonsurgical and surgical treatments for individuals who have not found relief elsewhere.
Montefiore Einstein is ranked in the top 1% of all hospitals in the nation for obstetrics and gynecology, urology care, and rehabilitation, according to U.S. News & World Report.
Our specialists have unparalleled expertise in emerging medical and noninvasive therapies, advanced laparoscopic and robot-assisted procedures, nerve-sparing techniques and fertility-preserving innovations—providing the latest minimally invasive approaches to diagnose and treat pelvic pain at its source. From initial evaluation to long-term management, we prioritize shared decision-making and are committed to relieving pain, restoring pelvic, sexual, reproductive and urinary function, and improving quality of life for each patient. Whether you have been experiencing chronic pelvic pain or are just beginning to seek answers for unexplained symptoms, we understand the challenges you may face and are here to help every step of the way.
Leaders in Advanced Diagnostics & Image-Guided Treatments
Montefiore Einstein earned the prestigious Diagnostic Imaging Center of Excellence (DICOE) designation from the American College of Radiology (ACR)—the highest level of achievement for medical imaging. We are also accredited by the American Institute of Ultrasound in Medicine (AIUM), demonstrating that we meet or exceed nationally recognized standards for the performance and interpretation of diagnostic obstetric and gynecologic ultrasound examinations—and underscoring our commitment to clinical excellence and the highest quality of care.

Advanced Diagnostics & Treatments
We provide access to the latest diagnostics and most advanced treatments to help restore quality of life for individuals living with pelvic pain.
Our Program offers state-of-the-art diagnostic technologies—including high-resolution 3T pelvic magnetic resonance imaging (MRI), diagnostic laparoscopy with pain mapping and real-time, high-definition hysteroscopy. For patients with bladder-related symptoms, we provide advanced cystourethroscopy techniques and multichannel video urodynamic studies, offered conveniently on-site at Montefiore Einstein Urogynecology and Reconstructive Pelvic Surgery. Our comprehensive diagnostic approach enables us to pinpoint the underlying causes of pelvic pain and create individualized treatment plans.
Nonsurgical treatments options include nutritional therapy, advanced hormonal and nonhormonal medical management, targeted neuropathic pain therapies, bladder instillations for interstitial cystitis and specialized pelvic floor physical therapy focused on restoring function and alleviating pain. We offer trigger point injections both in-office and in the operating room to alleviate abdominal and pelvic floor pain, and provide peripheral nerve blocks—including pudendal nerve blocks—for patients experiencing pudendal nerve pain and neuropathic pelvic pain. To further enhance recovery, we emphasize opioid-sparing multimodal analgesia, combining advanced pain management strategies to reduce opioid reliance. Behavioral health support is also integrated into our care model, addressing the emotional and mental health needs associated with chronic pelvic pain.
We offer the full range of minimally invasive surgical interventions including, MRI-guided focused ultrasound surgery (MRgFUS), uterine artery embolization and radiofrequency ablation for fibroid-related pain. We also provide neuromodulation therapies including sacral neuromodulation (Axonics®, InterStim®) and pudendal nerve neuromodulation for patients with complex pelvic pain syndromes, as well as emerging approaches such as dorsal root ganglion (DRG) stimulation for select refractory cases.
When surgical intervention is required, our multidisciplinary team specializes in the most advanced minimally invasive techniques—including laparoscopic, robot-assisted, hysteroscopic and vaginal approaches—designed to promote faster recovery, preserve fertility when appropriate and optimize long-term outcomes. Surgical procedures include laparoscopic fertility-sparing and nerve-sparing endometriosis surgery, laparoscopic and robot-assisted myomectomy for fibroids and minimally invasive or robot-assisted hysterectomy.
Our team provides specialized care for the full range of pelvic pain conditions, offering advanced diagnostics and therapies, including:
We provide access to the latest diagnostics to identify the root causes of pelvic pain with precision. Our diagnostic technologies include:
- Colonoscopy and sigmoidoscopy as needed
- Diagnostic hysteroscopy (real-time, high-definition visualization)
- Diagnostic laparoscopy with pain mapping
- Diagnostic nerve blocks (e.g. sacral nerve root anesthesia)
- High-resolution 3T pelvic MRI with endometriosis protocol
- Laboratory testing (e.g. complete blood count—CBC, thyroid, hormonal panels, sexually transmitted disease—STD screening, lactate dehydrogenase—LDH isoenzymes)
- MRI neurography for nerve entrapment syndromes
- Pelvic floor evaluation (electromyography—EMG, ultrasound, manual assessment)
- Saline infusion sonohysterography (SIS)
- 3D and 4D transvaginal and transabdominal pelvic ultrasound
- Urodynamic testing and multichannel video studies
Our wide range of hormonal and nonhormonal medical therapies are evidence-based and tailored to each patient’s symptoms and life stage.
- Hormonal therapies (e.g. oral contraceptives, intrauterine devices—IUDs, gonadotropin-releasing hormone—GnRH agonists/antagonists, selective progesterone receptor modulators—SPRMs, aromatase inhibitors)
- Neuropathic pain agents (e.g. gabapentin, serotonin–norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen
- Nutrition therapy (e.g. Vitamin B and magnesium to relieve dysmenorrhea)
- Opioid-sparing multimodal analgesia protocols
We offer a full spectrum of image-guided and energy-based procedures, neuromodulation and pain-focused therapies, including:
- Acupuncture
- Bladder instillations for interstitial cystitis
- Botox® injections (for pelvic floor muscle spasm and bladder-related pelvic pain)
- Cognitive behavioral therapy (CBT) and pain psychology
- Dorsal root ganglion (DRG) stimulation (for refractory pelvic pain)
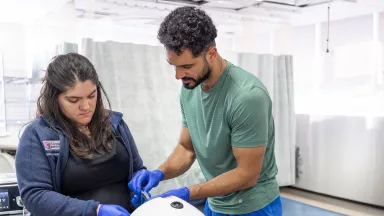
- Emsella chair (high intensity focused electromagnetic—HIFEM treatment for pelvic floor strengthening)
- Endometrial ablation (e.g. radiofrequency, cryoablation, thermal balloon)
- Integrated behavioral health support and psychological counseling
- Magnetic resonance-guided focused ultrasound surgery (MRgFUS)
- Office and operating room (OR)-based trigger point injections
- Peripheral nerve blocks (e.g. pudendal, ilioinguinal, genitofemoral nerves, sacral, hypogastric or ganglion impar)
- Physical therapy
- Pelvic floor physical therapy (manual therapy, biofeedback)
- Radiofrequency ablation (RFA)
- Laparoscopic radiofrequency ablation (Acessa® procedure)
- Transcervical fibroid ablation (Sonata® System)
- Sacral neuromodulation (InterStim®)
- Shockwave therapy (for myofascial pelvic pain)
- Transcutaneous nerve stimulation
- Ultrasound-guided high-intensity focused ultrasound (HIFU)
- Uterine artery embolization (UAE)
We are committed to innovation and to advancing the field of pelvic pain care, offering:
- Platelet-rich plasma (PRP) injections
- Stem cell therapy
We specialize in advanced minimally invasive surgery, with a focus on fertility preservation, nerve-sparing techniques and enhanced recovery. Our surgical offerings include:
- Endometriosis surgery
- Fertility-sparing endometriosis surgery
- Laparoscopic and/or robot-assisted excision of endometriosis
- Nerve-sparing endometriosis surgery
- Hysterectomy
- Laparoscopic supracervical hysterectomy
- LESS hysterectomy
- Robot-assisted laparoscopic hysterectomy
- Total laparoscopic hysterectomy
- Vaginal hysterectomy
- vNOTES hysterectomy
- Laparoscopic adhesiolysis
- Myomectomy (fibroid removal)
- Abdominal (open) myomectomy
- Hysteroscopic myomectomy (transcervical resection of fibroids)
- Laparoendoscopic single-site (LESS) myomectomy
- Laparoscopic myomectomy
- Robot-assisted laparoscopic myomectomy
- Vaginal natural orifice transluminal endoscopic surgery (vNOTES) myomectomy
- Nerve procedures
- Pudendal nerve decompression
Research & Clinical Trials
We are leading collaborative research and spearheading numerous studies and clinical trials, including several funded by the National Institutes of Health (NIH), translating novel scientific discoveries into new diagnostics and treatments to help improve clinical outcomes. Through our clinical trials, our patients can access emerging technologies and innovative treatments that may otherwise be unavailable to the general public.
Our pelvic pain research program is committed to advancing the understanding, diagnosis and treatment of a wide range of complex pelvic pain conditions. Our research spans basic, translational and clinical science, with a focus on investigating the underlying mechanisms of pelvic pain, including neuropathic signaling, visceral cross-sensitization and pelvic floor dysfunction. We are also developing and evaluating novel diagnostic tools, minimally invasive therapies and fertility-sparing treatment strategies.
In partnership with Montefiore Einstein Urology, our researchers are exploring the underlying mechanisms and pathophysiology of pelvic floor disorders, including bladder pain syndrome and overactive bladder. Through NIH grants, we are also studying the role of neuron-satellite glia cell signaling in pelvic pain and visceral cross-sensitization.
We are advancing the clinical management of symptomatic fibroids through ongoing research, including innovations and updates in uterine artery embolization techniques for the treatment of leiomyomas. Our team evaluated national contemporary treatment patterns among women diagnosed with symptomatic uterine fibroids in the United States, contributing valuable insights into current clinical practice. We also contributed to the development of the American Association of Gynecologic Laparoscopists (AAGL) endometriosis classification—a new anatomy-based surgical complexity score designed to more reliably differentiate levels of surgical complexity and inform clinical decision-making.
Our researchers are also exploring the clinical applications of emerging minimally invasive approaches, such as vNOTES, and developing novel surgical technologies and techniques to improve perioperative outcomes. Ongoing initiatives also focus on the evaluation and implementation of enhanced recovery after surgery (ERAS) protocols to optimize postoperative recovery and patient outcomes.

Care Navigation & Support Services
Whether you have been experiencing chronic pelvic pain, facing symptoms that remain unexplained, or are just beginning to seek answers—our world-renowned team at the Montefiore Einstein Pelvic Pain Program is here to provide you with exceptional support, care and resources tailored to your needs.
Our full-service Center offers a comprehensive range of traditional and holistic care at every stage of life from screening, prevention and diagnosis through treatment and recovery, including social and support services, genetic counseling and education, care navigation, mental health and wellness services, and other supportive programs. Our expansive breadth of resources enables us to deliver highly specialized and coordinated care that takes into account the whole person, addressing each individual’s complex medical needs to improve outcomes, relieve pain, restore pelvic, sexual and urinary function, and improve quality of life for each woman across every stage of life. Our team of compassionate and deeply knowledgeable doctors, nurses, specialists and support staff is dedicated to helping you at every step of your pelvic pain journey.
Your Pelvic Pain Program Team
Our multidisciplinary team of world-renowned gynecologists collaborates closely with specialists in urology, urogynecology and pelvic reconstructive surgery, reproductive endocrinology and infertility, gastroenterology, pain management, physical therapy, interventional radiology, behavioral health and other disciplines—specialize in diagnosing and managing the full range of pelvic pain conditions while addressing the complex, multifactorial nature of pelvic pain. We use the latest diagnostics and leading-edge therapies, delivering comprehensive, individualized care to relieve pain, restore pelvic, sexual, reproductive and urinary function, and improve each patient’s quality of life.
About Pelvic Pain
Pelvic pain is a complex and often debilitating condition frequently misunderstood, underdiagnosed or dismissed. It can present as acute or chronic, cyclical or constant, and may stem from a wide range of gynecologic, urologic, gastrointestinal, musculoskeletal or neurologic causes. Pelvic pain can interfere with daily activities, sexual health and overall quality of life. Since it often involves overlapping systems and conditions, effective care requires a nuanced and multidisciplinary approach.
Pelvic pain can be acute—beginning suddenly—or chronic, lasting for six months or longer. Common types of pelvic pain include dysmenorrhea (painful menstruation), dyspareunia (pain during or after sexual intercourse), noncyclical pelvic pain (unrelated to the menstrual cycle), ovulation-related pain (mittelschmerz), pain with bowel movements or urination and pelvic floor muscle pain (pelvic myalgia).
Chronic pelvic pain may result from one or more underlying conditions. It is often associated with a range of comorbid conditions, such as endometriosis, irritable bowel syndrome (IBS), bladder pain syndrome (interstitial cystitis), pelvic adhesions, musculoskeletal injuries, fibromyalgia, chronic central pain syndrome, anxiety and major depressive disorder.
Accurate diagnosis is essential—and often the first step toward meaningful relief. Evaluation typically begins with a comprehensive history and physical examination and may include advanced imaging, diagnostic procedures and targeted assessments of the pelvic floor and reproductive, genitourinary, gastrointestinal and neurologic systems. Treatment is often tailored to addressing each individual’s symptoms and underlying causes, integrating multimodal therapies such as medical management, physical therapy, minimally invasive procedures, behavioral health support and surgery when needed.
Managing chronic pelvic pain may require lifelong, individualized care. Without appropriate evaluation and treatment, it can lead to significant morbidity. However, with timely diagnosis and a comprehensive, multidisciplinary management approach, many individuals can experience meaningful symptom relief, improved or restored function and enhanced quality of life.
Conditions We Treat
Understanding the potential underlying causes of chronic pelvic pain—whether gynecologic, urologic, gastrointestinal, musculoskeletal, neurologic, biopsychosocial or multifactorial—is critical to effective detection, management and development of a tailored treatment strategy. We offer comprehensive diagnostic evaluation and multidisciplinary care for a wide range of conditions that contribute to pelvic pain, including:
- Chronic constipation
- Colorectal carcinoma
- Inflammatory bowel disease (IBD)
- Irritable bowel syndrome (IBS)
- Abnormal uterine bleeding
- Adenomyosis
- Chronic pelvic inflammatory disease (PID)
- Dysmenorrhea (painful periods)
- Endometriosis
- Gynecologic cancer
- Hydrosalpinx
- Ovarian cysts
- Ovarian remnant syndrome
- Pelvic adhesions (scar tissue)
- Pelvic floor disorders (e.g. pelvic organ prolapse)
- Peripartum pelvic pain syndrome
- Post tubal ligation pain syndrome
- Uterine fibroids
- Vulvodynia
- Coccygodynia
- Fibromyalgia
- Low back pain (e.g. lumbar disc herniation)
- Myofascial pain syndrome
- Pelvic floor muscle spasm
- Central nervous system hypersensitivity (central sensitization syndrome)
- Complex regional pain syndrome
- Nerve entrapment syndromes (e.g. ilioinguinal, genitofemoral, obturator nerve)
- Neuropathic pelvic pain
- Peripheral neuropathy
- Pudendal neuralgia
- Postsurgical pelvic pain
- Psychological and behavioral factors (e.g. anxiety and depression impacting pain perception)
- Sexual dysfunction
- Bladder cancer
- Bladder pain syndrome (interstitial cystitis)
- Chronic urethritis
- Kidney stones
- Neurogenic bladder
- Recurrent urinary tract infections
- Urinary incontinence
- Pelvic congestion syndrome
- Vulvar varicosities