Our Approach to Lower Anogenital Tract Disease





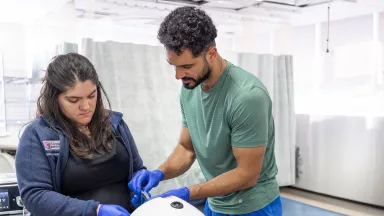
Montefiore Einstein’s Lower Anogenital Tract Disease Management Program is an internationally recognized leader, providing comprehensive, state-of-the art care for those with lower anogenital tract neoplasia or are at risk. Our multidisciplinary team includes world-renowned gynecologic oncologists who collaborate closely with medical and radiation oncologists, infectious disease and human immunodeficiency virus (HIV) specialists, colorectal surgeons and others to deliver seamless, coordinated care and ensure the best possible outcomes for every patient.
Integrating the latest techniques and technologies available, our research-driven, individualized approach emphasizes HPV and cancer screening, prevention and risk reduction through advanced precancer detection and treatment, lifestyle modification and HPV vaccination when appropriate. We’re ranked in the top 1% of all hospitals in the nation for obstetrics and gynecology and cancer care and are among the highest performing hospitals in the nation for gynecologic cancer surgery, according to U.S. News & World Report. Our Gynecologic Oncology Program is also fully integrated with our National Cancer Institute (NCI)-designated Montefiore Einstein Comprehensive Cancer Center—among the elite 1% of NCI-designated comprehensive cancer centers in the U.S.
As one of the few programs of its kind in the nation, we serve as an international referral center for the most complex and rare lower anogenital tract cases. Our team provides specialized expertise in advanced screening and diagnostic techniques and offers access to leading-edge HPV testing platforms, including both Food and Drug Administration (FDA)-approved and investigational self-collection-based sampling methods. Our specialists use the most advanced and newly emerging treatments for the full range of anogenital tract diseases—from office-based therapies such as topical agents and precision excisional procedures to advanced radiation and systemic therapies, as well as complex surgical interventions. We prioritize minimally invasive, robot-assisted and fertility-sparing approaches whenever appropriate. Through our clinical trials, patients also have access to innovative diagnostics and novel therapies that may not be available to the general public.
Our Program is centered on long-term wellness and cancer prevention, and emphasizes patient education and shared decision-making—empowering individuals to take an active role in managing their lower anogenital health. Whether you’re undergoing evaluation for abnormal Papanicolaou (Pap) or HPV test results, managing a diagnosis of dysplasia or cancer, recovering from treatment or seeking preventative care, our team is here to provide expert guidance and comprehensive support at every stage of your anogenital health journey.
Access to the Most Advanced Testing Available
Our Program provides convenient access to the most advanced screening, diagnostics and treatments for lower anogenital tract diseases, including expert colposcopy and high-resolution anoscopy (HRA). We offer the latest FDA-approved highly sensitive HPV tests that allow for self-collection in a clinical setting as well as investigational at-home self-collected HPV testing through our participation as one of the lead sites in the NCI 'Last Mile' Initiative which supports the Self-collection for HPV testing to Improve Cervical Cancer Prevention (SHIP) Trial Network. We also offer the only FDA-approved p16/Ki-67 dual-stain triage test for HPV-positive cervical cancer screening results as well as extended HPV genotyping to risk stratify and more efficiently triage patients for colposcopy.

Advanced Diagnostics & Treatments
We offer access to the most advanced diagnostic technologies and innovative treatments for the prevention, early detection and management of the full range of lower anogenital tract conditions—including cervical, vaginal, vulvar and anal dysplasia and cancers. Many evaluations and procedures are performed in-office, providing patients with seamless, efficient and compassionate care.
Depending on the diagnosis, we offer a full range of personalized, leading-edge nonsurgical and surgical treatments, including targeted therapies tailored to the type, stage and severity of the disease—as well as to each individual’s unique needs, lifestyle, preferences and goals. When clinically appropriate, lifestyle modification and HPV vaccination are incorporated as part of a preventative and therapeutic strategy.
Our suite of advanced diagnostics and treatments include:
We offer access to the most advanced screening and diagnostic techniques and technologies, including:
- Advanced imaging
- Computed tomography (CT)
- High-resolution 3T magnetic resonance imaging (MRI) of the pelvis
- Intravenous pyelogram (IVP)
- Positron emission tomography (PET) scans
- 3D and 4D pelvic ultrasound
- Adjunctive laboratory and molecular diagnostics
- Immunohistochemistry (e.g. p16 and Ki-67 as biomarkers) to confirm dysplasia
- p16/Ki-67 dual-stain triage test (CINtec® PLUS Cytology) for HPV-positive cervical cancer screening results
- Experimental/research-based testing
- Cervical and anal swab-based microbiome analysis
- DNA methylation markers (e.g. CADM1, MAL, FAM19A4)
- HPV E6/E7 protein assays
- HPV integration site analysis
- HPV viral load quantification
- Next-generation sequencing (NGS) for HPV variants and subtypes
- Immunohistochemistry (e.g. p16 and Ki-67 as biomarkers) to confirm dysplasia
- Clinical evaluation
- Bimanual pelvic examination
- Comprehensive medical, surgical, gynecologic, sexual and HPV-related history
- Digital anal rectal examination (DARE)
- Pain and sensory testing (when indicated for differential diagnosis of overlapping conditions such as vulvodynia)
- Pelvic exam with speculum inspection
- Visual inspection of vulva, perineum, perianal area and cervix
- Colposcopy: a specialized procedure using a magnifying instrument under light illumination to examine the cervix, vagina and vulva
- Cervical colposcopy
- Vaginal colposcopy (vaginoscopy): colposcopic evaluation of the vaginal walls without a speculum
- Vulvar colposcopy (vulvoscopy): colposcopic examination of the vulva
- Cystoscopy (for bladder involvement)
- Digital and photographic tools
- Digital photography integration for documentation and follow-up (e.g. digital cervicography)
- Endocervical curettage
- High-resolution anoscopy (HRA): a specialized procedure using an anoscope and high-resolution microscope to visualize the anal canal and perianal area
- HPV testing
- Cotesting (Pap test and HPV molecular test)
- HPV-based testing includes primary HPV testing alone or co-testing (Pap test plus HPV molecular test)
- Molecular testing:
- High-risk HPV deoxyribonucleic acid (DNA) testing (detects the presence of DNA from high-risk HPV types)
- HPV genotyping (provides type-specific identification for HPV 16, 18, etc.)
- HPV messenger ribonucleic acid (mRNA) testing (detects E6/E7 viral mRNA, indicating active viral replication)
- Reflex and triage testing
- HPV tests used in response to abnormal cytology or for post-treatment surveillance
- Post-colposcopy or post-treatment follow-up
- Reflex cytology
- Reflex genotyping
- Reflex testing for atypical squamous cells of undetermined significance (ASC-US) cytology or a positive primary HPV screening test
- Triage testing of low-grade squamous intraepithelial lesion (LSIL) or atypical glandular cells (AGC) results
- Self-collected HPV testing
- At-home self-collection (investigational as part of the NCI ‘Last Mile’ Initiative)
- FDA-approved HPV tests that allow for self-collection in a clinical setting
- Other infectious disease testing
- HIV and sexually transmitted infection (STI) screening
- Pap test to detect cytologic abnormalities
- Anal Pap
- Cervical Pap
- Proctoscopy (for rectal and anal canal visualization)
- Targeted biopsies
- Colposcopy with biopsy
- HRA with biopsy
- Targeted tissue sampling from abnormal areas seen on colposcopy or HRA
Advanced Treatment
- HPV vaccination
- GARDASIL® 9 (HPV 9-valent vaccine, recombinant) which protects against nine HPV types
- Lifestyle modification and smoking cessation
- Observation and surveillance
- Topical treatments and medical therapies
- Cidofovir gel: antiviral (investigational/compassionate use)
- 5-Fluorouracil (5-FU): topical chemotherapy agent
- Imiquimod (Aldara): topical immune response modifier
- Photodynamic therapy
- Systemic antivirals or immunotherapy
- Trichloroacetic acid (TCA): chemical ablation
- Ablative therapies
- Cryotherapy (e.g. liquid nitrogen)
- Laser ablation (CO₂ laser or Nd:YAG)
- Thermal ablation (e.g. cold coagulation, diathermy)
- Electrosurgery
- Electrocautery
- Fulguration
- Hyfrecation
- Expedited approaches
- Excisional treatments (conization)
- Cold-knife conization
- HRA-guided or colposcopy-guided excision
- Large loop excision of the transformation zone (LLETZ)
- Laser therapy (laser cone biopsy)
- Loop electrosurgical excision procedure (LEEP)
- Skinning vulvectomy
- Ultrasound surgical aspiration
- Anal surgery
- Local resection (including sphincter-sparing techniques) and abdominoperineal resection (APR)
- Fertility-sparing options
- Cervical conization, simple or radical trachelectomy (for cervical cancer)
- Hysterectomy
- Simple or radical hysterectomy, with lymphadenectomy if indicated
- Laparoscopic or robot-assisted
- Local excision
- Wide local excision (WLE)
- Laser or scalpel excision of lesions
- Minimally invasive and robot-assisted approaches are prioritized whenever appropriate
- Pelvic exenteration (for advanced or recurrent disease)
- Reconstructive surgery (as needed post-excision)
- Vaginectomy (with or without lymphadenectomy)
- Partial, total or radical vaginectomy
- Vulvectomy
- Simple, partial or radical vulvectomy
- HPV vaccination
- Fertility preservation counseling
- Palliative care
- Pelvic floor physical therapy
- Psychosocial support and mental health counseling
- Sexual health counseling
- Regular follow-up
- HPV testing and cytology
- Imaging (MRI, PET/CT) for advanced disease monitoring
- Re-excision or retreatment for recurrent dysplasia
- Repeat colposcopy or HRA
Research & Clinical Trials
We are leading collaborative research and spearheading numerous studies and clinical trials, including several funded by the National Institutes of Health (NIH), translating novel scientific discoveries into new diagnostics and treatments to help improve clinical outcomes. Through our clinical trials, our patients can access emerging technologies and innovative treatments that may otherwise be unavailable to the general public.
Our researchers actively lead basic, translational and clinical investigations to advance the understanding, diagnosis and treatment of lower anogenital tract diseases. We are leading research focused on human papillomavirus (HPV) and HPV-related cancers—from elucidating how HPV affects cellular function and the molecular mechanisms of viral integration and oncogenesis to developing next-generation diagnostics and treatments. These include novel therapeutic HPV vaccines aimed at preventing and treating cervical, vulvar, vaginal and anal cancers. We are also at the forefront of innovation in screening technologies, driving research on primary HPV testing and other emerging technologies for early cervical cancer detection.
Our researchers are leading studies that address cervical cancer prevention and management in women living with human immunodeficiency virus (HIV) and treatment of anal high-grade squamous intraepithelial lesions (HSIL) to prevent anal cancer. In addition, we’re researching new ways to treat primary and recurrent cervical cancer with proton radiation therapy in collaboration with the New York Proton Center, the only proton facility in New York State.

Care Navigation & Support Services
Whether you’re undergoing evaluation for abnormal Pap or HPV test results, managing a diagnosis of dysplasia or cancer, recovering from treatment or seeking preventative care, our world-renowned team at the Montefiore Einstein Lower Anogenital Tract Disease Management Program is here to provide you with exceptional support, care and resources tailored to your needs.
Our full-service program offers a comprehensive range of traditional and holistic care at every stage of life from screening, prevention and diagnosis through treatment and recovery. We offer integrated services including social and support programs, genetic counseling and education, care navigation, mental health and wellness support and personalized programs designed to meet each individual’s unique needs.
Our breadth of resources enables us to deliver highly specialized and coordinated care that takes into account the whole person, addressing each individual’s medical needs to optimize outcomes, prevent, eliminate or control cancer, alleviate symptoms, prevent recurrence and promote, preserve and restore the reproductive and sexual health of women across every stage of life. Our team of compassionate and deeply knowledgeable doctors, nurses, specialists and support staff is dedicated to helping you at every step of your anogenital health journey.
At the Forefront of Early Cancer Detection
At the Montefiore Einstein Lower Anogenital Tract Disease Management Program, we are committed to preventing cancer and ensuring that everyone has access to the most advanced testing to help detect cancer early and save lives.
Learn about our state-of-the-art, patient-friendly screening methods, designed to reduce your cancer risk and detect cancer at the earliest most treatable stage, even before symptoms appear.
Your Lower Anogenital Tract Disease Management Team
Our multidisciplinary team includes world-renowned gynecologic oncologists who collaborate closely with medical and radiation oncologists, infectious disease and HIV specialists, colorectal surgeons and other experts who deliver comprehensive, individualized care for the full range of lower anogenital tract diseases. We are committed to delivering the highest quality, patient-centered care, with a focus on early detection, risk reduction and evidence-based strategies to prevent, eliminate or control cancer, alleviate symptoms, prevent recurrence and enhance quality of life.
About Lower Anogenital Tract Diseases
Lower anogenital tract diseases encompass a spectrum of precancerous and cancerous conditions characterized by abnormal cell changes in the tissues of the cervix, vagina, vulva and anus—most often caused by persistent infection by high-risk types of human papillomavirus (HPV). These diseases include dysplasia, or intraepithelial neoplasia, which may progress to invasive cancer without careful monitoring and treatment. Risk factors for developing these diseases include HPV infection (especially high-risk strains), a history of lower anogenital tract dysplasia or cancer, immunosuppression (including HIV infection or prior solid organ transplantation), smoking and a history of lower genital tract precancerous lesions. While early-stage dysplasia is often asymptomatic, progression can lead to abnormal bleeding, pain and visible or palpable lesions. Routine screening is essential for early detection and effective intervention. Advances in HPV testing, cytology, colposcopy, HRA and targeted therapies can allow for earlier detection, minimally invasive treatment and improved outcomes—especially when integrated into comprehensive, individualized care plans.
Conditions We Treat
Dysplasia refers to the presence of abnormal cells within a tissue or organ. While it is not cancer, dysplasia is considered a precancerous condition which has the potential to develop into cancer over time if left untreated.
- Cervical intraepithelial neoplasia (CIN)
- Cervical low-grade squamous intraepithelial lesion (LSIL): CIN 1
- Cervical high-grade squamous intraepithelial lesion (HSIL): CIN 2/3
- Vulvar intraepithelial neoplasia (VIN)
- Vulvar LSIL: VIN 1
- Vulvar HSIL: VIN 2/3
- Vaginal intraepithelial neoplasia (VAIN)
- Vaginal LSIL: VAIN 1
- Vaginal HSIL: VAIN 2/3
- Anal intraepithelial neoplasia (AIN)
- Anal LSIL: AIN 1
- Anal HSIL: AIN 2/3
- Cervical cancer
- Squamous cell carcinoma
- Adenocarcinoma
- Adenosquamous (mixed) carcinoma
- Clear cell adenocarcinoma
- Neuroendocrine tumors (small cell and large cell cervical cancer)
- Vulvar cancer
- Squamous cell carcinoma
- Basal cell carcinoma
- Melanoma
- Paget disease
- Verrucous carcinoma
- Bartholin’s gland adenocarcinoma
- Sarcoma
- Vaginal cancer
- Squamous cell carcinoma
- Adenocarcinoma
- Sarcoma
- Melanoma
- Small cell carcinoma
- Lymphoma
- Anal cancer
- Squamous cell carcinoma
- Adenocarcinoma
- Melanoma
- Multifocal HPV-related lower anogenital tract cancers
- High-risk HPV infection
- Persistent HPV infection with abnormal cytology
- Genital warts (condyloma acuminata)
- HPV infection, especially high-risk strains
- History of lower anogenital tract precancerous lesions or dysplasia
- History of lower anogenital tract cancer
- Immunosuppression (including HIV infection or prior solid organ transplant)
- Smoking (tobacco use)
- Sexual activity (such as multiple partners or early onset of sexual activity)
- History of anogenital warts (condyloma acuminata)
Learn More About Lower Anogenital Tract Neoplasia Screening, Prevention & Treatment
Receiving a precancer or cancer diagnosis or being at risk for or suspected of having cancer can feel overwhelming, but learning about the diagnosis can help you navigate treatment and care. Visit the links below to learn about some of the different types of anogenital tract neoplasias, their causes and associated symptoms, as well as screening, diagnosis, prevention and treatment options. Schedule a consultation with us for diagnosis, prevention and treatment options for these or any other types of gynecologic precancers or cancers.
Tumor Boards
Our multidisciplinary team of world-renowned gynecologic oncologists, medical and radiation oncologists, colorectal surgeons and HIV and infectious disease specialists collaborates closely across disciplines, developing comprehensive and personalized treatment plans tailored for each patient. Through our multidisciplinary tumor boards, we review each patient’s case, medical history and treatment options in detail before recommending a comprehensive, personalized treatment plan and identifying patients who are candidates for our clinical trials.