Our Approach to Reproductive Endocrinology & Infertility





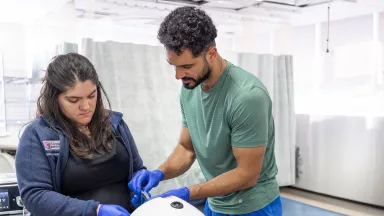
One of the most recognized assisted reproductive technology (ART) programs in Westchester County, the Bronx and the lower Hudson Valley, the Montefiore Einstein Institute for Reproductive Medicine and Health (MIRMH) is a premier full-service destination and one of the only fertility centers in New York City offering the complete range of state-of-the-art medical, surgical and procedural fertility options for individuals and couples seeking to build or expand their families. Our Institute brings together a multidisciplinary team of world-renowned experts in reproductive endocrinology and infertility (REI), maternal-fetal medicine, reproductive genetics, advanced imaging and embryology to provide comprehensive, individualized care for anyone facing fertility challenges. Our advanced programs and innovative services address the full range of reproductive endocrine conditions and both female and male causes of infertility—including ovulatory dysfunction, tubal and uterine factors, male factor and unexplained infertility, genetic conditions, polycystic ovary syndrome (PCOS), premature ovarian insufficiency (POI), hormonal imbalances, male hypogonadism (low testosterone), menopause and recurrent pregnancy loss.
Our Institute is the only one of its kind in the region offering on-site physician care, surgical care, a full-service in vitro fertilization (IVF) lab and laboratory services seamlessly integrated in one location.
We use the latest and most advanced reproductive testing and treatments and specialize in minimally invasive fertility-sparing procedures and preservation techniques—with IVF success rates exceeding the national average. Whether you have been trying to conceive without success, are managing a complex reproductive health condition or are exploring fertility preservation, we are committed to optimizing each individual’s chance of pregnancy, delivering expert care at every stage of the reproductive journey.
In addition, our experts in reproductive endocrinology specialize in optimizing the management of menopausal symptoms, bone health and ovulatory or abnormal uterine bleeding dysfunction related to hormones. They work closely with each patient to provide an optimal individualized plan tailored to their care goals and fertility needs.
Our world-renowned multidisciplinary team of board certified physicians offers unparalleled expertise across the full spectrum of fertility care—from medical management cycles to IVF. We take the time to thoroughly evaluate each patient’s medical history, diagnostic findings and prior treatments before recommending a personalized care plan. While IVF can offer high success rates, it is not always necessary. Whenever appropriate, we begin with less invasive, more affordable treatments tailored to each individual’s unique needs. Our use of all available treatment options reflects our commitment to providing the highest quality, evidence-based care with compassion and individualized support at every stage of the reproductive journey.
Our Center is open 365 days a year and performs egg retrievals on-site at our Westchester County location, including weekends. Patients may also complete blood work, ultrasounds and other diagnostic procedures with us on Saturdays and Sundays—offering scheduling flexibility and continuity of care not typically available at other centers. Additionally, we coordinate IVF cycles with outside facilities for routine monitoring, such as bloodwork and ultrasounds, when preferred or clinically indicated.
Our internationally recognized physicians are distinguished leaders in the field, having trained and mentored generations of REI specialists around the world. While many centers routinely recommend or require intracytoplasmic sperm injection (ICSI) and preimplantation genetic testing for aneuploidy (PGT-A) for all patients undergoing IVF, our physicians use an evidence-based, personalized approach, guiding collaborative treatment planning tailored to each individual’s needs. We offer fertility treatments that may not be available at many other centers, including ovulation induction cycles with or without intensive monitoring, laparoscopic procedures such as myomectomy and tubal repair and hysteroscopic tubal cannulation. Our patient-centered treatment protocols are also designed to minimize medication costs and reduce the number of injections required, helping to expand access to fertility care for all who seek it.
Our on-site laboratories perform thousands of tests and procedures each year with a focus on the highest standards of safety, accuracy, and identity protection. We combine extensive resources, a highly trained team, and leading-edge research to support a safe and healthy pregnancy for each patient. Our state-of-the-art laboratories undergo rigorous inspections for quality assurance and control, and are accredited, certified and licensed by numerous accrediting and regulatory agencies such as Clinical Laboratory Improvement Amendments (CLIA), the New York State Department of Health, the U.S. Food and Drug Administration (FDA), and the College of American Pathologists (CAP)—the global standard for quality and performance and the highest accreditation standard in IVF laboratory practice. Our lab is an active member of the Society of Assisted Reproductive Technology (SART), with team members holding leadership roles in the society.
State-of-the-Art Programs
Montefiore Einstein Reproductive Endocrinology & Infertility is a premier full-service destination, providing comprehensive, innovative care for the full range of reproductive endocrine conditions and both female and male causes of infertility. Explore our comprehensive suite of state-of-the-art programs below.
Our ART Program offers comprehensive infertility evaluations, preconception testing and optimization and a full range of leading-edge fertility treatments, including advanced fertility-optimizing surgeries and procedures.
Our Program provides comprehensive evaluation and personalized management for individuals experiencing early miscarriage or repeated pregnancy loss.
Our Program offers comprehensive cryopreservation services—including egg, sperm and embryo freezing—for individuals seeking to preserve their reproductive potential prior to medical treatments such as cancer therapy, other fertility-impacting interventions or for future family building.
In collaboration with Montefiore Einstein Reproductive and Medical Genetics, our Program offers comprehensive preimplantation genetic testing (PGT) services, including PGT for a monogenic disorder (PGT-M), PGT for aneuploidy (PGT-A) and PGT for structural chromosome rearrangements (PGT-SR).
Our comprehensive Reproduction Preservation Program offers a full range of options—including donor eggs, sperm and embryos, as well as gestational carriers—to assist individuals and couples in building their families through assisted reproductive technologies. We were among the first in New York State to establish a donor egg program. Egg donation may be recommended for those facing reproductive or fertility challenges such as advanced maternal age, premature ovarian insufficiency, diminished ovarian reserve, a history of unsuccessful IVF cycles, an elevated risk of inherited genetic conditions or prior medical or surgical treatments affecting fertility.

Advanced Diagnostics & Treatments
We offer access to the most advanced diagnostics and treatments available, ensuring the highest quality care for individuals and couples navigating complex reproductive or endocrine barriers to conception. Our team performs comprehensive diagnostic evaluations, including advanced imaging, to accurately identify the underlying causes of reproductive endocrine conditions and infertility in both women and men—essential for developing effective, personalized treatment plans.
We offer preconception counseling and evaluation and comprehensive fertility testing using state-of-the-art screening and diagnostic technologies. Our services include advanced laboratory testing such as hormonal and endocrine blood testing as well as the latest genetic testing with next generation sequencing to evaluate inherited conditions that may cause infertility or recurrent pregnancy loss.
For female fertility evaluation, we provide sophisticated imaging—including 3D and 4D transvaginal and transabdominal ultrasounds, saline infusion sonohysterograms (SIS) and hysterosalpingograms to assess uterine and tubal anatomy. We also specialize in hysteroscopy to directly visualize and manage structural abnormalities of the uterus.
For male fertility evaluation, we offer advanced scrotal ultrasound to assess for varicoceles, testicular masses and other conditions; transrectal ultrasound for evaluation of ejaculatory ducts, seminal vesicles and prostate; and comprehensive semen analysis for sperm health evaluation.
Advanced endocrine treatments, including the latest hormone therapies, endocrine-modulating therapies and corticosteroids, are used to manage hormonal imbalances that affect fertility, menstrual function, pregnancy maintenance, menopause symptoms, as well as bone and cardiovascular health. We also offer the full range of the most advanced fertility treatments available today, including IVF, ICSI and intrauterine insemination (IUI), as well as medications and surgery to treat various causes of reproductive endocrine disorders and infertility. Our embryology team brings unmatched expertise, offering advanced PGT, time-lapse imaging and morphokinetic analysis for IVF and sophisticated blastocyst biopsy to enable accurate embryo diagnostics and optimize reproductive outcomes.
We specialize in minimally invasive fertility-sparing procedures for women and men, including egg, sperm and embryo cryopreservation, particularly in patients preparing for cancer treatment or with other conditions that affect fertility. We provide novel minimally invasive solutions, including advanced laparoscopic, hysteroscopic, vaginal and robotic surgery, to address a wide range of common and complex conditions that may cause infertility, such as fibroids, endometriosis and polycystic ovarian syndrome, for faster recovery and less pain. We also offer surgical approaches to sperm extraction.
At the Forefront of Reproductive Medicine
Our on-site laboratory services span the complete range of diagnostic and therapeutic testing and technologies for the treatment of the full range of reproductive endocrine conditions and both male and female causes of infertility. Our fertility and embryology laboratory is recognized as one of the leading laboratories in New York for andrology, embryology and endocrine testing—delivering exceptional accuracy, innovation and the highest quality patient care. All of our laboratories, along with our operating and recovery rooms, are all in one location. This integration allows for minimized wait times, seamless coordination and a unique opportunity for patients to engage directly with laboratory staff. Our board certified experts educate each patient on every step of the process, providing regular progress updates in a supportive and collaborative environment. We offer the full range of advanced diagnostics and treatments and andrology, embryology and endocrine services, including:
Includes the diagnosis and treatment of conditions related to male reproductive and sexual health conditions and male fertility.
- Advanced sperm testing (including deoxyribonucleic acid—DNA fragmentation testing, oxidative stress testing, sperm chromatin structure assays)
- Comprehensive semen analysis (assessment of sperm count, volume, viscosity, pH, motility, morphology and vitality)
- Genetic testing (e.g. karyotype analysis, Y-chromosome microdeletion testing, cystic fibrosis transmembrane conductance regulator—CFTR gene mutation analysis, single gene or panel testing)
- Hormonal testing (e.g. testosterone, follicle-stimulating hormone—FSH, luteinizing hormone—LH, prolactin levels)
- Post-ejaculatory urinalysis (if azoospermia and retrograde ejaculation is suspected)
- Scrotal and transrectal ultrasound for evaluation of varicoceles, testicular masses, epididymal pathology and ejaculatory duct obstruction
- Sperm cryopreservation for patients preparing for cancer treatment or with other conditions that affect fertility
- Sperm processing for IUI or IVF (e.g. sperm washing, density gradient centrifugation)
- Storage of cryopreserved donor sperm
- Surgical sperm retrieval (including testicular sperm extraction—TESE and percutaneous epididymal sperm aspiration—PESA)
- Treatment of varicoceles and erectile or ejaculatory dysfunction
- Diagnostic testing
- Anti-Müllerian hormone (AMH)
- Androgens (total and free testosterone, dehydroepiandrosterone sulfate—DHEA-S)
- FSH, LH, estradiol
- Insulin, fasting glucose, HbA1c (to assess insulin resistance and PCOS)
- Midluteal phase progesterone level, LH surge testing, ovulation tracking
- Pregnancy tests
- Prolactin
- Thyroid function tests
- Advanced endocrine treatments
- Endocrine treatments—including the latest hormone therapies, endocrine-modulating therapies and corticosteroids—are used to manage hormonal imbalances that affect fertility, menstrual function, pregnancy maintenance, as well as bone and cardiovascular health.
- Anti-androgen therapy: for management of androgen excess in PCOS
- Corticosteroid therapy: for adrenal insufficiency or autoimmune-related reproductive endocrine dysfunction
- Endocrine-modulating therapies: such as dopamine agonists for hyperprolactinemia
- Estrogen and progesterone therapy: for conditions such as POI, menopause and hypothalamic amenorrhea
- Gonadotropin therapy: for ovulation induction or spermatogenesis (e.g., in Kallmann syndrome or other causes of gonadotropin deficiency)
- Hormone replacement therapy (HRT): for conditions such as Turner syndrome and menopause
- Pulsatile GnRH therapy: for hypogonadotropic hypogonadism in men and women to stimulate FSH and LH secretion
- Testosterone therapy: for male hypogonadism (low testosterone)
- Thyroid hormone therapy: for hypothyroidism affecting reproductive health
- Endocrine treatments—including the latest hormone therapies, endocrine-modulating therapies and corticosteroids—are used to manage hormonal imbalances that affect fertility, menstrual function, pregnancy maintenance, as well as bone and cardiovascular health.
- In vitro fertilization (IVF)
- Artificial insemination through intracytoplasmic sperm injection (ICSI)
- Assisted hatching
- Blastocyst transfer
- Cryopreservation (sperm, egg—oocyte, embryo freezing and storage)
- Donor eggs/egg donation
- Donor sperm/sperm donation
- Egg retrieval
- Embryo transfer (fresh embryo transfer, frozen embryo transfer—FET, single embryo transfer—SET, multiple embryo transfer—MET, blastocyst-stage—day 5 or 6—embryo transfer, cleavage-stage—day 2 or 3—embryo transfer, donor embryo transfer)
- Fertilization
- Gestational carrier
- Intrauterine insemination (IUI)
- In vitro maturation (IVM)
- Ovulation stimulation through injections or pills
- Testicular sperm extraction (TESE)
- Preimplementation genetic testing (PGT)
- Preimplantation genetic testing for a monogenic disorder (PGT-M), previously known as preimplementation genetic diagnosis (PGD)
- Preimplantation genetic testing for aneuploidy (PGT-A), previously known as Preimplementation genetic screening (PGS)
- Preimplantation genetic testing for structural chromosome rearrangements (PGT-SR)
- Cervical cerclage to treat or prevent cervical insufficiency
- Oncofertility surgery in individuals undergoing treatment for cancer, such as gynecologic cancer and testicular cancer
- Fertility-sparing surgeries for gynecologic cancers such as radical trachelectomy for cervical cancer and unilateral salpingo-oophorectomy or cortical sparing surgery for ovarian tumors
- Testis-sparing surgery for testicular cancer, nerve-sparing retroperitoneal lymph node dissection (RPLND) and sperm retrieval and cryopreservation
- Ovarian function preservation procedures such as ovarian tissue cryopreservation, ovarian cystectomy, ovarian transposition (oophoropexy)
- Sperm, egg or embryo cryopreservation before gonadotoxic treatments
- Surgical sperm retrieval such as testicular sperm extraction (TESE) and percutaneous epididymal sperm aspiration (PESA)
- Surgery for endometriosis and pelvic pain, often performed using minimally invasive techniques, with same-day discharge home following the procedure
- Testis-sparing surgery
- Transurethral resection of ejaculatory ducts (TURED)
- Tubal surgery such as laparoscopic surgery to open fallopian tubes (salpingostomy), removal of adhesions (adhesiolysis) and reversal of tubal ligation
- Uterine surgery
- Uterine fibroid surgery including myomectomy (fibroid removal using a hysteroscopic, laparoscopic or abdominal approach), uterine artery embolization, magnetic resonance-guided focused ultrasound surgery (MRgFUS) and radiofrequency ablation––RFA (laparoscopic RFA or ultrasound-guided transcervical RFA)
- Hysteroscopic surgery for correction of intrauterine abnormalities and optimization of the uterine environment for conception (such as hysteroscopic resection of a uterine septum or removal of intrauterine adhesions)
- Varicocelectomy (surgical repair of varicocele)
- Vasovasostomy (vasectomy reversal)
Research
We are leading collaborative research and spearheading numerous studies and clinical trials, including several funded by the National Institutes of Health (NIH). Through our clinical trials, our patients can access emerging technologies and innovative treatments that may otherwise be unavailable to the general public.
Some of the main areas of research are focused on exploring the underlying mechanisms of infertility and menopause, advancing fertility preservation and fertility treatments, studying the development of reproductive disorders, human endometrial maturation, the effect of obesity and weight loss on reproductive function, investigating new causes and prevention of pregnancy loss and micro ribonucleic acids (microRNAs) as gene regulators in endometrial function.
Our researchers have made numerous seminal contributions to the field, including identifying that colony-stimulating factor 1 (CSF-1) signaling is essential for preimplantation development and defining the mechanism of how progesterone negatively regulates estrogen-induced uterine epithelial cell proliferation and preparing the uterus for blastocyst implantation.
We are studying the function of nucleolar channel systems (NCSs) in human reproduction. These micron-sized membranous organelles are implicated in the preparation of the endometrium for uterine attachment of the fertilized egg and the timing of embryo transfer in IVF cycles to boost IVF success rates. Our researchers also recently developed a personalized prediction model of live birth after IVF in women with PCOS.
We are also conducting numerous large-scale Society for Assisted Reproductive Technology Clinic Outcome Reporting System studies. We conducted the largest study to date, analyzing clinical and neonatal outcomes between frozen and fresh oocytes after fresh embryo transfer, in both donor and autologous oocyte cycles. We conducted the first and largest study to use the Society for Assisted Reproductive Technology (SART) national registry to understand the clinical implications of using ICSI stratified by type of embryo transfer (fresh, frozen-thawed with PGT and frozen-thawed without PGT) and whether ICSI is indicated.

Care Navigation & Support Services
Whether you have been trying to conceive without success, managing a complex reproductive health condition or exploring fertility preservation, our world-renowned team at Montefiore Einstein Reproductive Endocrinology and Infertility is here to provide you with exceptional support, care and resources tailored to your needs.
Our full-service center offers a comprehensive range of traditional and holistic care across the full range of reproductive health—from screening, prevention and diagnosis to treatment and recovery. This includes social and support services, genetic counseling and education, care navigation, mental health and wellness services and other personalized programs to meet the unique needs of each individual. Our expansive breadth of resources enables us to deliver highly specialized and coordinated care that takes into account the whole person, addressing each individual’s complex medical needs to improve outcomes and promote, preserve and restore reproductive and sexual health across every stage of life. Our team of compassionate and deeply knowledgeable doctors, nurses, specialists and support staff is dedicated to helping you at every step of your reproductive care journey.
Your Reproductive Endocrinology & Infertility Team
Our multidisciplinary team of world-renowned board certified obstetricians and gynecologists includes fellowship-trained experts in REI, providing comprehensive, state-of-the-art care for the full range of reproductive endocrine conditions and both male and female causes of infertility. We are committed to preserving fertility and optimizing each individual’s chance of pregnancy—delivering expert care at every stage of the reproductive journey. These leaders in reproductive endocrinology can assist with improving menopause-related concerns, including bone health and treatment options.
About Reproductive Endocrine Conditions & Infertility
Reproductive endocrine conditions and causes of infertility encompass a broad range of disorders that affect hormone regulation, reproductive health, and the ability to conceive. These conditions may involve the hypothalamic-pituitary-gonadal axis—the hormonal pathway that regulates reproduction—as well as ovarian or testicular function, or structural abnormalities of the reproductive tract. Infertility may result from female factors—such as ovulatory dysfunction, tubal disease, or uterine abnormalities—male factors such as low testosterone or abnormal semen parameters, or may be unexplained. In females, common reproductive endocrine concerns include polycystic ovary syndrome (PCOS), menstrual irregularities, endometriosis, uterine anomalies such as fibroids or Asherman’s syndrome, primary ovarian insufficiency (POI), and menopause-related hormonal changes. In males, conditions such as hypogonadism and other hormonal imbalances may affect sperm production or function. Hormonal disorders, including thyroid dysfunction and hyperprolactinemia, can also impact fertility. Genetic and hereditary conditions—such as Turner syndrome, Klinefelter syndrome, Fragile X premutation, and POI—are associated with increased risks for infertility, recurrent pregnancy loss, or transmission of inherited conditions. Comprehensive care—including early diagnosis, coordinated multidisciplinary management, and personalized treatment that may combine medical, surgical, and lifestyle approaches—is essential to identifying underlying causes, optimizing fertility, enhancing quality of life, and supporting lifelong reproductive health and family-building goals.
Conditions We Treat
We treat the full range of reproductive endocrine conditions as well as female and male causes of infertility, including:
- Adolescent reproductive endocrine disorders (e.g. delayed puberty, congenital reproductive anomalies)
- Endometriosis (e.g.. persistent pelvic pain related to hormones)
- Fertility preservation for cancer patients (e.g. egg, sperm and embryo freezing)
- Genetic or hereditary conditions (e.g. Turner syndrome, Klinefelter syndrome, Fragile X premutation carriers, primary ovarian insufficiency which are associated with an increased risk for infertility, recurrent pregnancy loss or transmission of heritable genetic conditions)
- Hormonal disorders affecting reproduction (e.g. thyroid dysfunction, hyperprolactinemia)
- Infertility (e.g. female factor infertility, including ovulatory dysfunction and tubal and uterine factors, male factor infertility and unexplained infertility)
- Male reproductive endocrine disorders (e.g. hypogonadism—low testosterone, sperm abnormalities)
- Menopause and bone health (e.g. osteoporosis)
- Menstrual irregularities (e.g. heavy bleeding, amenorrhea, oligomenorrhea)
- Ovulatory disorders (e.g. anovulation, irregular menstrual cycles)
- Polycystic ovary syndrome (PCOS)
- Primary ovarian insufficiency (POI)
- Recurrent pregnancy loss
- Uterine abnormalities (e.g. fibroids, congenital anomalies, Asherman’s syndrome)
Our Location
Institute for Reproductive Medicine and Health