Physical Medicine & Rehabilitation Research

Science at the Heart of Physical Medicine & Rehabilitation
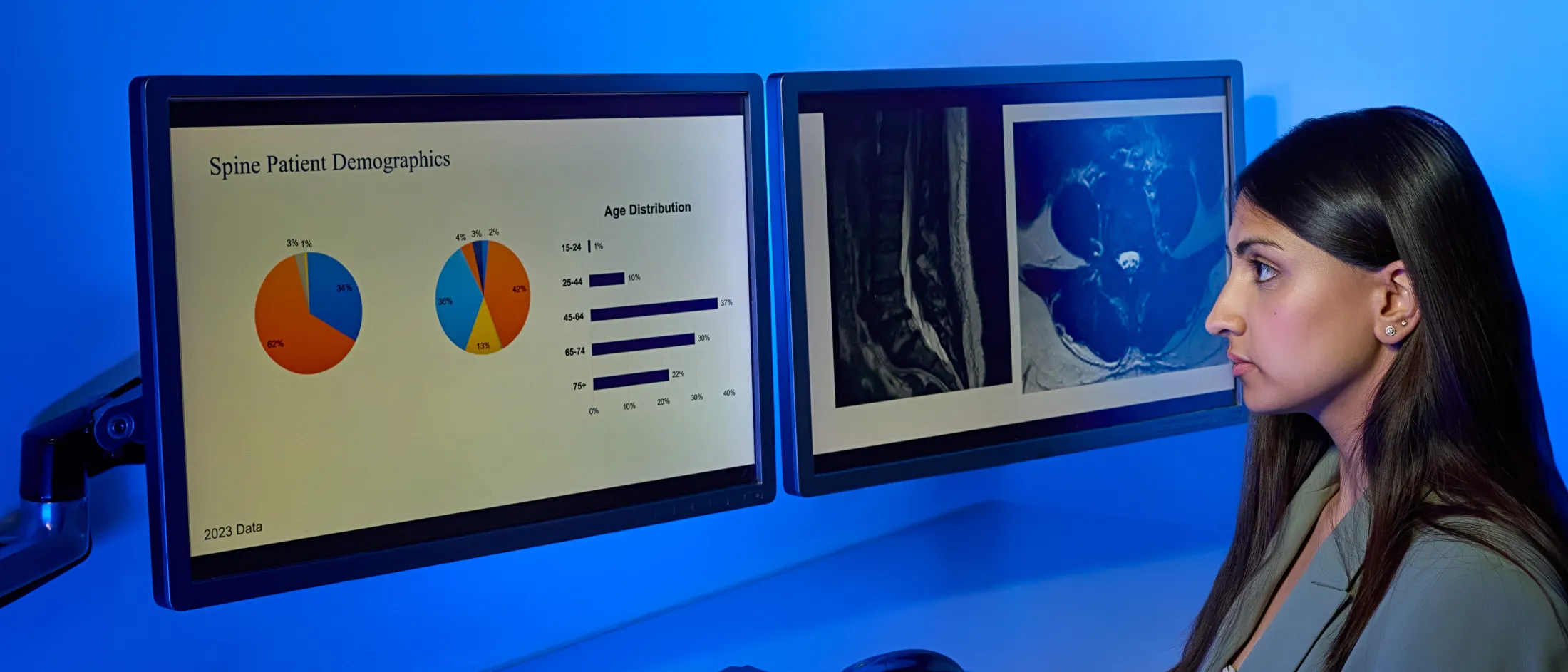
The Department of Physical Medicine and Rehabilitation is dedicated to advancing knowledge and treatment for individuals with disabilities, pain and impaired function. Our internationally recognized physician-scientists and biomedical investigators collaborate with both industry and federal support, spearheading numerous clinical trial initiatives and basic and translational research projects.
Our projects focus on restoring function and improving the quality of life for all our patients. We use advanced technologies, such as three-dimensional (3D) printing and applications, to deliver care in the home or offer low-cost solutions adaptable to diverse settings. Our research also includes implantable technologies for pain management and assessing stroke recovery.
We are committed to education in research and involve trainees at various levels, from high school and college students to medical students, residents and fellows in our projects. We invite you to explore our studies and reach out if you are interested in participating as a researcher or participant in our various trials.
Published Research
Association of Academic Physiatrists Residency and Fellowship Program Directors’ Resident Recruitment Subcouncil Position Paper on Residency Recruitment
Dragojlovic N, Romanoski N, Bolger A, Friedlander T, Helkowski W, Huss SA, Jenkins JG, Knowlton T, Nguyen DH, Rand SE, Raum G, Sullivan W, Tonkin B, Escalon MX
Description
This position paper represents a consensus document developed by the Association of Academic Physiatrists Residency and Fellowship Program Directors Council to address significant changes in physical medicine and rehabilitation residency recruitment practices. The study design employed a comprehensive literature review methodology conducted by a multidisciplinary workgroup comprising program directors, program coordinators, residents and medical students. The authors examined the evolution of residency recruitment from traditional in-person interviews to fully virtual formats, identifying both positive and negative downstream effects. These included decreased costs for applicants and programs, reduced time away from clinical activities, increased scheduling flexibility, but also increased application volume for both candidates and programs. The paper synthesizes available data from the Association of American Medical Colleges and provides evidence-based best practices for program leaders and applicants navigating this transformed recruitment landscape, emphasizing the need for standardized approaches to virtual recruitment processes that maintain the quality of candidate assessment while addressing the challenges of remote evaluation.
Trainee Insight into Pain Fellowship Programs: A Critical Evaluation of the Current Educational System by the APPD
Wahezi S, Naeimi T, Caparo M, Emerick T, Choi H, Eshraghi Y, Anitescu M, Patel K, Przkora R, Wright T, Moeschler S, Barad M, Rand S, Oh-Park M, Seidel B, Yener U, Alerte J, Shaparin N, Kaye A, Kohan L
Description
This cross-sectional survey study employed an online questionnaire methodology to investigate trainees’ motivations, expectations and perspectives regarding pain medicine fellowship programs across the United States. The study design used SurveyMonkey to target pain fellowship applicants in 2023 and current fellows, with surveys disseminated through residency and fellowship program directors to their trainees. The research yielded 283 survey participants, comprising 80% applicants in residency training and 20% current fellows, representing a convenience sampling approach that may limit generalizability. The findings revealed that participants ranked basic interventional procedures and the desire to learn advanced procedures as the most significant factors in pursuing pain fellowships, with 70% of trainees opposed to extending fellowship duration to two years and 50% expressing interest in private practice careers. The study highlighted important gaps in the current educational model, with participants emphasizing procedural volume and diversity as critical factors while rejecting extended training duration. This suggests that program directors need to develop innovative strategies to maintain competitive applicant interest while adapting to the evolving field of pain medicine.
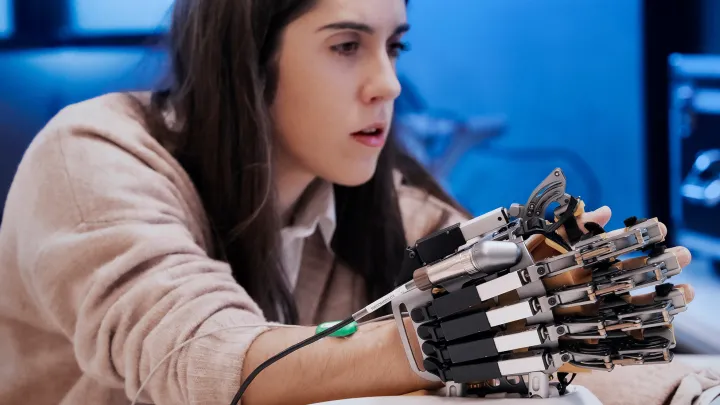
Approaches to Prosthetic Limb Restoration in Resource-Limited Settings/Countries
Rand S, Suprameni T, Bartels MN, Gitkind A
Description
This narrative review article examines the application of three-dimensional (3D) printing technology for prosthetic limb restoration in resource-limited developing countries, addressing a critical gap in accessible prosthetic care. The study design employed a comprehensive literature review methodology to analyze the potential of 3D printing to overcome traditional barriers in prosthetic fabrication, including high costs, limited manufacturing efficiency and lengthy production times. The authors explored how 3D printing technology can reduce prosthetic production time by approximately 86.2% and decrease costs by 88% compared to traditional methods, while enabling customization to meet individual patient needs. The review highlighted the transformative impact of additive manufacturing in enhancing prosthetic functionality, patient satisfaction and overall care delivery efficiency, while acknowledging challenges such as the need for specialized expertise and initial infrastructure investments. The paper demonstrated how digital fabrication technologies can extend traditional socket fabrication processes, potentially increasing the number of patients treated in rehabilitation clinics in low-resource areas by reducing time to completion and improving access to prosthetic services.
Yoga and Physical Therapy for Chronic Pain and Opioid Use Disorder Onsite in an Opioid Treatment Program: A Randomized Controlled Trial
Groeger JL, Perez HR, Moonaz S, Bartels MN, Rand S, Ghiroli MM, Zhang C, Bao Y, Gabbay V, Estremera GV, Bryant G, Hidalgo J, Hribar MB, Rodgers CRR, Savitzky J, Stein MR, Uebelacker LA, Starrels JL, Nahvi S
Description
This study represents a hybrid type-1 effectiveness-implementation randomized controlled trial designed to address the lack of integrated treatment for chronic pain and opioid use disorder (OUD). The study design employs a three-arm randomized controlled trial methodology where 345 participants with chronic low back pain and OUD from opioid treatment programs in the Bronx, NY, will be randomly assigned to 12 weeks of on-site yoga, on-site physical therapy or treatment as usual in a 1:1:1 allocation ratio. The primary outcomes include pain intensity measured by numerical rating scales, opioid use quantification and cost-effectiveness analysis, while secondary outcomes encompass physical function and overall well-being measures. The innovative study design tests a patient-centered approach to combined management of chronic pain and OUD by delivering nonpharmacological interventions directly on-site at opioid treatment programs, thereby removing traditional barriers to accessing these therapeutic modalities. This pragmatic trial design addresses real-world implementation challenges while rigorously examining the efficacy of yoga and physical therapy as cost-effective treatments for individuals facing barriers to integrated care, potentially providing evidence for widespread dissemination of these interventions to reduce pain, decrease opioid use and improve quality of life.
Adult Ankle Fractures (Ankle and Foot Soft Tissue Injuries and Fractures)
Shane Mario André Drakes, MD, Anusha Lekshminarayanan, MD, Petra Aboulhosn, MD
Description
This educational resource represents a comprehensive clinical review and knowledge synthesis focused on adult ankle fractures and associated soft tissue injuries within the context of physical medicine and rehabilitation (PM&R) practice. The publication employs a clinical practice guideline methodology, synthesizing current evidence-based approaches to ankle fracture management from a rehabilitation medicine perspective. Dr. Shane Mario André Drakes, serving as Program Director for the Sports Medicine Fellowship at Montefiore Einstein, brings specialized expertise in nonsurgical treatment of musculoskeletal injuries, using ultrasound technology for injury evaluation and procedural guidance. The review covers comprehensive assessment and treatment approaches for adult ankle fractures, incorporating both acute management principles and rehabilitation considerations essential for physiatrists managing these common orthopedic injuries. The publication is designed as an educational tool for PM&R Knowledge Now®. It provides evidence-based recommendations for clinical practice that integrate injury prevention, diagnostic approaches and treatment modalities specific to the rehabilitation medicine specialty, reflecting Dr. Drakes’ clinical focus on injury epidemiology, prevention strategies and evidence-based treatment recommendations for musculoskeletal conditions.
Multidisciplinary Collaborative Guidance on the Assessment and Treatment of Patients with Long Covid: A Compendium Statement
Cheng AL, Herman E, Abramoff B, Anderson JR, Azola A, Baratta JM, Bartels MN, Bhavaraju-Sanka R, Blitshteyn S, Fine JS, Fleming TK, Verduzco-Gutierrez M, Herrera JE, Karnik R, Kurylo M, Longo MT, McCauley MD, Melamed E, Miglis MG, Neal JD, Oleson CV, Putrino D, Rydberg L, Silver JK, Terzic CM, Whiteson JH, Niehaus WN
Description
This comprehensive guidance document represents a multidisciplinary consensus statement developed by the American Academy of Physical Medicine and Rehabilitation’s Multi-Disciplinary Post-Acute Sequelae of SARS-CoV-2 Infection Collaborative using a modified Delphi methodology. The collaborative comprises over 40 long COVID centers and includes physiatrists, primary care physicians, pulmonologists, cardiologists, psychiatrists, neuropsychologists, neurologists, occupational therapists, physical therapists, speech-language pathologists, patients and government representatives. The guidance establishes long COVID as an infection-associated chronic condition affecting at least 6% of the global population, with higher prevalence among females, certain racial/ethnic groups and nonurban residents, though anyone can develop long COVID regardless of initial COVID-19 test status. The document provides a holistic clinical framework emphasizing symptom-based supportive care, energy conservation strategies and careful attention to postexertional malaise/symptom exacerbation, while acknowledging significant unknowns in the field. The comprehensive approach addresses assessment protocols, treatment recommendations delivered with clinical humility, workplace accommodation strategies and disability considerations under the Americans with Disabilities Act, representing the most current evidence-based guidance for managing this complex, multisystem condition that closely resembles other infection-associated chronic conditions such as myalgic encephalomyelitis/chronic fatigue syndrome.
Clinical Outcomes of a New Foot-Worn Non-Invasive Biomechanical Intervention Compared to Traditional Physical Therapy in Patients With Chronic Low Back Pain. A Randomized Clinical Trial
Veeramachaneni R, Gitkind A, Yerra S, Hagan M, Hasanoglu AN, Akile N, Kareff H, Ho D, Bartels MN
Description
This randomized controlled trial employed a 2:1 allocation ratio comparing a personalized home-based biomechanical intervention (HBBI, AposHealth) to traditional physical therapy in 162 patients with chronic low back pain. The study design used a linear mixed model to assess changes over time across baseline, 12-week and 52-week follow-up visits, with the primary outcome measure being pain intensity using a standard numeric rating scale at 52 weeks. Secondary outcomes included comprehensive pain and function metrics, quality of life measures and objective spatio-temporal gait testing. The results demonstrated significant superiority of the HBBI intervention, with participants showing a marginal mean reduction of 3.5 points in pain scores (from 6.2 to 2.7, representing a 56% reduction) compared to traditional physical therapy participants who achieved a mean decrease of 1.8 points (from 6.9 to 5.1, representing a 26% reduction). The study represents an important advancement in nonpharmacological, nonsurgical interventions for chronic nonspecific low back pain, demonstrating that innovative foot-worn biomechanical interventions can provide clinically meaningful improvements in pain management and may serve as an effective adjunct to current standard of care approaches for this prevalent condition affecting quality of life and functional capacity.
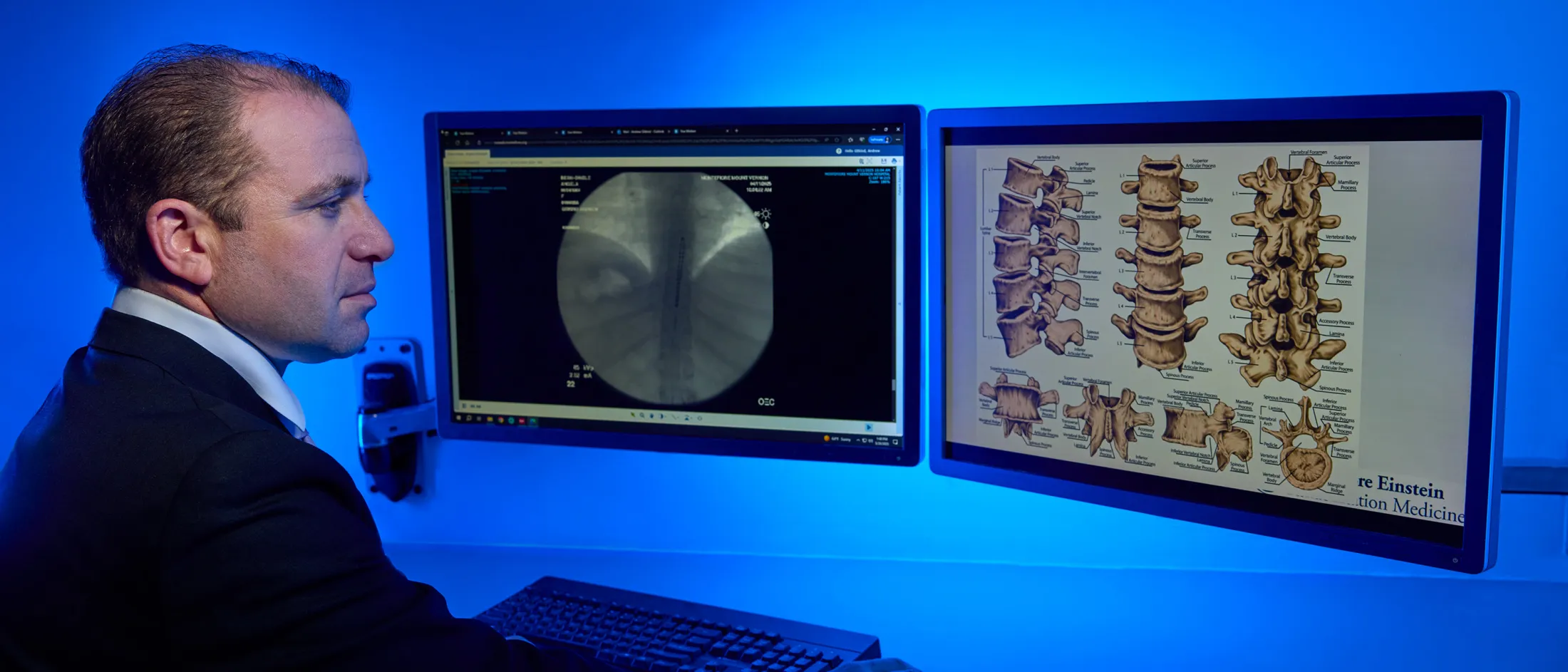
Spinal Cord Stimulation Explantation and Chronic Pain: A Systematic Review and Technology Recommendations
Wahezi SE, Yener U, Naeimi T, Lewis JB, Yerra S, Sgobba P, Ciftci HB, Vydyanathan A, Chiu E, Cherkalin D, Darji JY, Masterson R, Lee D, Jarusriwanna A, Palee S, Ortiz NR, Caparo M, Dayon E, Fontaine C, Bikson M, Schatman ME, Pritzlaff SG, Deer TR, Hunter CW
Description
This systematic review employed three primary screening methods, including manual search with keywords, Medical Subject Headings (MeSH) term queries and reference list screening across PubMed, Cochrane and Web of Science databases from inception to November 2024. The methodology involved independent reviewers conducting data extraction with second reviewer verification and discrepancy resolution by the corresponding editor, ultimately analyzing 25 studies from an initial yield of 719 articles. The review examined data from 13,026 patients who underwent permanent spinal cord stimulation implantation between 1984 and 2024, identifying that 1,882 patients (9.82%) required explantation. The primary reasons for explantation were lack of efficacy and inadequate pain relief (38%), followed by lead failure (15%) and infection (14%), with most explantations occurring within the first year despite spinal cord stimulation being generally safe and effective. The study addresses critical concerns about device durability and cost-effectiveness in the context of chronic pain affecting 20.5% of the U.S. population and costing $296 billion annually in lost productivity, highlighting the need for improved patient selection criteria and technological innovation to address the current hardware-driven model that limits waveform flexibility, particularly given the substantial implantation costs ($35,000–$70,000) and revision costs ($15,000–$25,000) that raise payor concerns.
Employer Perspective on Pain Fellowship Education: A Survey to Understand the Current State of Pain Medicine Training
Wahezi SE, Yener U, Naeimi T, Choi H, Eshraghi Y, Pritzlaff SG, Emerick T, Hunter CW, Caparo M, Schatman ME, Ahadian F, Argoff C, Deer T, Sayed D, Day M, Abd-Elsayed A, Lo Bianco G
Description
This national survey study used a cross-sectional methodology distributed through multiple professional pain organizations, including the American Academy of Pain Medicine, American Society of Interventional Pain Physicians, North American Neuromodulation Society and American Society of Pain and Neuroscience, as well as the Pain DocMatters forum. The study collected 196 responses (39 from Pain DocMatters and 157 through society channels) from pain physician employers representing diverse geographic locations, practice types and clinical settings. The results revealed a critical gap in pain medicine fellowship training, with only 7% of respondents feeling that fellows were adequately prepared for independent practice following the current one-year Accreditation Council for Graduate Medical Education (ACGME)-approved fellowship model. Employers identified professionalism and basic interventional skills as the most highly valued attributes, with spinal cord stimulator (SCS) trials ranked as the most important advanced procedure for trainees to master, followed by SCS implants, peripheral nerve stimulator (PNS) implants, interspinous spacers and percutaneous vertebral procedures. The overwhelming majority of respondents indicated that fellows require additional training beyond graduation to practice independently, highlighting the need for pain medicine education programs to provide more robust training to meet the evolving demands of the field and emerging technologies, thereby better preparing graduates for the complexity of contemporary pain medicine practice.
The Current State of Training in Pain Medicine Fellowships: An Association of Pain Program Directors (APPD) Survey of Program Directors
Wahezi SE, Emerick TD, Caparó M, Choi H, Eshraghi Y, Naeimi T, Kohan L, Anitescu M, Wright T, Przkora R, Patel K, Lamer TJ, Moeschler S, Yener U, Alerte J, Grandhe R, Bautista A, Spektor B, Noon K, Reddy R, Osuagwu UC, Carpenter A, Gerges FJ, Horn DB, Murphy CA, Kim C, Pritzlaff SG, Marshall C, Kirchen G, Oryhan C, Swaran Singh TS, Sayed D, Lubenow TR, Sehgal N, Argoff CE, Gulati A, Day MR, Shaparin N, Sibai N, Dua A, Barad M
Description
This survey study employed a three-phase recruitment methodology (advanced notification, invitation and follow-up) targeting 56 program directors of ACGME-accredited pain fellowship programs across the United States, achieving a 69% response rate (39/56 program directors). The study design used a standardized online questionnaire covering clinical experience, interventional training, subcategory fields, online educational platforms, postgraduate practice success and training adequacy. The research revealed significant challenges in providing comprehensive training within the current 12-month fellowship structure, with all program directors allowing fellows to participate in industry-related and professional society procedural workshops and 59% actively encouraging such participation. The findings demonstrated that 54% of program directors expressed the need to extend fellowship training duration to reduce reliance on supplemental education from industry or professional pain societies. Program directors emphasized integrity, professionalism and diligence as critical attributes for long-term success. They also acknowledged the fundamental challenge of adequately training fellows in all pain medicine subspecialties within the current timeframe. This has led to discussions about curriculum standardization and the potential need for extended training programs to ensure comprehensive competency development in the rapidly evolving field of pain medicine.
Case Report: The Successful Use of Hydroxyzine for Analgesia in a Patient With Lumbar Spinal Stenosis
Bhatta M, Dayon E, Martinez E, Bell E, Caparo M
Description
This case report employs a descriptive case study methodology following CARE guidelines to document the successful use of hydroxyzine, an H1 inverse agonist antihistamine, for pain management in a patient with lumbar spinal stenosis. The study presents a 51-year-old woman with low back pain radiating to the right lower extremity, diagnosed through magnetic resonance imaging (MRI) revealing multilevel degenerative changes, including bilateral foraminal narrowing at L5-S1 and ligamentous hypertrophy causing spinal stenosis. Despite conservative treatments failing to provide adequate relief, the administration of hydroxyzine 10 mg three times daily resulted in a clinically significant 50% reduction in reported pain on the numeric rating scale at three-month follow-up. The case report discusses potential mechanisms of action, including hydroxyzine's antagonistic effects on H1 receptors located on lumbar nerve roots and its interaction with neural cytokines, representing a novel therapeutic approach for neurogenic claudication. This rare documentation of antihistamine efficacy for spinal stenosis pain challenges conventional pain management paradigms and suggests the need for further clinical investigation into antihistamines as alternative or adjunctive treatment options for patients with lumbar spinal stenosis who are refractory to standard pain medications, spinal injections and surgical interventions.
Iliotibial Band Syndrome Current Evidence
Bonoan M, Morales M, Liu XW, Oyeniran O, Zheng K, Palatulan E
Description
This review article comprehensively examines the current understanding, diagnosis and management of iliotibial band (ITB) syndrome, a prevalent cause of lateral knee pain—particularly in runners and active individuals. The authors synthesize recent advances in the literature regarding epidemiology, pathophysiology, risk factors and clinical presentation of ITB syndrome, highlighting developments in imaging techniques and biomechanical considerations. Treatment modalities discussed range from conservative measures, such as physical therapy, activity modification and anti-inflammatory approaches, to more advanced interventions—including corticosteroid injections and, in rare cases, surgical procedures. The article also evaluates the effectiveness of preventative strategies and ongoing controversies regarding optimal management. With an evidence-based approach, the review provides physicians and rehabilitation specialists with up-to-date recommendations for both the acute and chronic stages of ITB syndrome, emphasizing a multidisciplinary strategy tailored to individual patient presentations.
Innovations and Next Steps in Adaptive and Para Sports
Cordova-Vallejos C, Tinney M, Palatulan E
Description
This narrative review explores recent advancements and future directions within the field of adaptive and para sports, drawing on emerging research and practical innovations that are shaping the participation and performance of athletes with disabilities. The article highlights technological developments in assistive devices, advancements in classification systems, improvements in athlete training protocols and enhanced accessibility in sports infrastructure. Additionally, the authors discuss the increasing emphasis on inclusion, policy evolution and the impact of global events, such as the Paralympic Games, in raising awareness and driving change. The review advocates for a multidisciplinary approach involving clinicians, coaches, engineers and policymakers to continue breaking down barriers for adaptive athletes. Concluding with key priorities for research and collaboration, the paper calls for sustained support and innovation to ensure equitable opportunities and holistic well-being for participants in para and adaptive sports worldwide.
Manuscript in review, BJSM Manuscript ID bjsports-2024-109125.R4
Mental Health in Adaptive and Para Athletes
Aboulhosn P, Giampaolo G, Aguilar J, Palatulan E
Description
This review article addresses the unique mental health challenges faced by adaptive and para athletes, synthesizing evidence from both clinical research and practice. The authors analyze psychosocial stressors associated with physical disability, high-level competition and the complex intersection of identity, stigma and resilience in para sport contexts. Attention is given to the prevalence and spectrum of mental health concerns such as anxiety, depression and adjustment disorders among this population, as well as protective factors including social support, self-advocacy and tailored coping strategies. The article evaluates current models for mental health screening and intervention within adaptive sports, emphasizing culturally sensitive approaches and the need for integrated care between mental health professionals, rehabilitation specialists and coaching staff. The review advocates for further research, targeted education and policy reforms to optimize mental health outcomes and athletic performance in adaptive and parasport settings.
Accepted and awaiting publication.
Your Generosity Makes a Difference
The Department of Physical Medicine and Rehabilitation is deeply committed to developing innovative solutions to optimize health, function and quality of life of individuals with physical and cognitive disabilities across the lifespan through clinical research, as well as teaching and mentoring the next generation of physician-scientists.




