Lung Cancer Screening
Finding lung cancer in its earliest stage offers the best chance of successful treatments. That’s why screening for lung cancer is important if you are at an increased risk.
Montefiore Einstein Comprehensive Cancer Center is passionate about routine screenings for those at risk for lung cancer and many other cancer types at our NCI-designated Center.
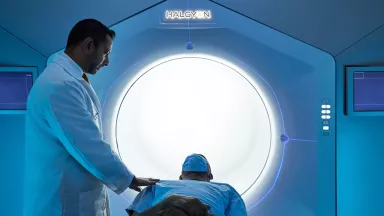
Our high-risk lung cancer screening program focuses on finding cancer as early as possible, even before symptoms occur, so you can take steps to protect your health. These screenings are essential to lung cancer prevention. The high-risk screening uses low-dose computed tomography (CT) scans to help detect the disease at its earliest, a method proven to reduce mortality due to lung cancer, compared with the standard chest x-ray. This program is the first of its kind in the Bronx, where the smoking rate is the second highest in New York City, at 16.2%. The program is offered to individuals who meet the criteria established in the landmark National Lung Screening Trial sponsored by the National Cancer Institute. Eligible patients must meet the following criteria:
- Between ages 50-80
- Have not had a chest CT scan in the previous year
- Smokes or is a former smoker who quit within the last 15 years
- Has smoked a minimum of 20 “pack years”; for example, one pack a day for 20 years or two packs a day for 10 years
At Montefiore Einstein Comprehensive Cancer Center, you can expect our compassionate and skilled healthcare providers to offer personalized screening in a supportive setting. And you’ll benefit from the latest, most advanced technology available to treat lung cancer as well as access to the latest in clinical trials.
The discovery of a lung nodule requires timely evaluation to ensure the best possible outcome. At Montefiore Einstein Comprehensive Cancer Center, the Follow-Up ASessmenT of Lung Nodules (FAST) Clinic is dedicated to providing rapid assessment, diagnosis, and treatment. With advanced technology—including a leading-edge robotic bronchoscopy suite—our team delivers fast, accurate care to help patients move forward with confidence.
For more than 50 years, Montefiore Einstein Comprehensive Cancer Center has been a leader in the research, diagnosis, and treatment of over 200 types of cancer. Turn to us for comprehensive cancer screening.

Cancer Clinical Trials
- Blood & Bone Marrow Cancers
- Brain, Spine & Central Nervous System Cancers
- Breast Cancer
- Childhood Cancers
- Endocrine System Cancers
- Gastrointestinal (GI) Cancers
- Genitourinary (GU) & Urologic Cancers
- Gynecologic Cancers
- Head & Neck Cancers
- Kaposi Sarcoma & AIDS-Related Cancers
- Lung & Chest Cancers
- Prostate Cancer
- Sarcomas
- Skin Cancer
As an NCI-designated comprehensive cancer center, Montefiore Einstein Comprehensive Cancer Center supports the mission and guidelines of the National Cancer Institute (NCI). The following information about types of cancer, prevention and treatments is provided by the NCI.
Lung Cancer Screening (PDQ®)–Patient Version
What Is Screening?
Screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
Scientists are trying to better understand which people are more likely to get certain types of cancer. They also study the things we do and the things around us to see if they cause cancer. This information helps doctors recommend who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarily think you have cancer if he or she suggests a screening test. Screening tests are given when you have no cancer symptoms.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
General Information About Lung Cancer
Key Points
- Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung.
- Lung cancer is the leading cause of cancer death in the United States.
- Different factors increase or decrease the risk of lung cancer.
Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung.
The lungs are a pair of cone-shaped breathing organs in the chest. The lungs bring oxygen into the body as you breathe in. They release carbon dioxide, a waste product of the body's cells, as you breathe out. Each lung has sections called lobes. The left lung has two lobes. The right lung is slightly larger, and has three lobes. A thin membrane called the pleura surrounds the lungs. Two tubes called bronchi lead from the trachea (windpipe) to the right and left lungs. The bronchi are sometimes also involved in lung cancer. Tiny air sacs called alveoli and small tubes called bronchioles make up the inside of the lungs.

Anatomy of the respiratory system showing the trachea, the right and left lungs and their lobes, and the bronchi. The lymph nodes and the diaphragm are also shown. Oxygen is inhaled into the lungs and passes through the alveoli (the tiny air sacs at the end of the bronchioles) and into the bloodstream (see inset), where it travels to the tissues throughout the body.
There are two main types of lung cancer: small cell lung cancer and non-small cell lung cancer.
Other PDQ summaries containing information related to lung cancer include:
Lung cancer is the leading cause of cancer death in the United States.
Lung cancer is the second most common type of non-skin cancer in the United States. Lung cancer is the leading cause of cancer death in men and in women.
Different factors increase or decrease the risk of lung cancer.
Anything that increases your chance of getting a disease is called a risk factor. Anything that decreases your chance of getting a disease is called a protective factor.
Tobacco smoking is the most important risk factor for lung cancer. Cigarette, cigar, and pipe smoking all increase the risk of lung cancer. Tobacco smoking causes about 9 out of 10 cases of lung cancer in men and about 8 out of 10 cases of lung cancer in women. The best way to prevent lung cancer is to not smoke.
For information about risk factors and protective factors for lung cancer, see Lung Cancer Prevention.
Lung Cancer Screening
Key Points
- Tests are used to screen for different types of cancer when a person does not have symptoms.
- Three screening tests have been studied to see if they decrease the risk of dying from lung cancer.
- Screening with LDCT scans has been shown to decrease the risk of dying from lung cancer in heavy smokers.
- Screening with chest x-rays and/or sputum cytology does not decrease the risk of dying from lung cancer.
- Screening tests for lung cancer are being studied in clinical trials.
Tests are used to screen for different types of cancer when a person does not have symptoms.
Scientists study screening tests to find those with the fewest harms and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) helps a person live longer or decreases a person's chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
Three screening tests have been studied to see if they decrease the risk of dying from lung cancer.
The following screening tests have been studied to see if they decrease the risk of dying from lung cancer:
- Low-dose computed tomography (LDCT): A procedure that uses low-dose radiation to make a series of very detailed pictures of areas inside the body using an x-ray machine that scans the body in a spiral path. This procedure is also called spiral scan or helical scan.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Sputum cytology: Sputum cytology is a procedure in which a sample of sputum (mucus that is coughed up from the lungs) is viewed under a microscope to check for cancer cells.
Screening with LDCT scans has been shown to decrease the risk of dying from lung cancer in heavy smokers.
The National Lung Screening Trial studied people aged 55 years to 74 years who had smoked at least 1 pack of cigarettes per day for 30 years or more. Participants were either current smokers or former smokers who had quit within the last 15 years. The trial used chest x-rays or LDCT scans to check for signs of lung cancer.
Screening with LDCT once a year for three years was better than chest x-rays at finding early-stage lung cancer and decreased the risk of dying from lung cancer in current and former heavy smokers.
Current smokers whose LDCT scan result shows possible signs of cancer may be more likely to quit smoking.
Screening with LDCT can cause possible harms, including:
- false-positive test results, which may lead to invasive procedures which are not needed
- overdiagnosis of some lung cancers, though it is not clear how often this happens
For more information about these possible harms, see the Risks of Lung Cancer Screening below.
A Guide is available for patients and doctors to learn more about the benefits and harms of screening for lung cancer.
Screening with chest x-rays and/or sputum cytology does not decrease the risk of dying from lung cancer.
Chest x-ray and sputum cytology are two screening tests that have been used to check for signs of lung cancer. Screening with chest x-ray, sputum cytology, or both of these tests does not decrease the risk of dying from lung cancer.
Screening tests for lung cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Risks of Lung Cancer Screening
Key Points
- Screening tests have risks.
- The risks of lung cancer screening tests include the following:
- Finding lung cancer may not improve health or help you live longer.
- False-negative test results can occur.
- False-positive test results can occur.
- Chest x-rays and CT scans expose the chest to radiation.
- Talk to your doctor about your risk for lung cancer and your need for screening tests.
Screening tests have risks.
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying from cancer.
The risks of lung cancer screening tests include the following:
Finding lung cancer may not improve health or help you live longer.
Screening may not improve your health or help you live longer if you have lung cancer that has already spread to other places in your body.
When a screening test result leads to the diagnosis and treatment of a disease that may never have caused symptoms or become life-threatening, it is called overdiagnosis. It is not known if treatment of these cancers would help you live longer than if no treatment were given, and treatments for cancer may have serious side effects. Harms of treatment may happen more often in people who have medical problems caused by heavy or long-term smoking.
False-negative test results can occur.
Screening test results may appear to be normal even though lung cancer is present. A person who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if there are symptoms.
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result (one that shows there is cancer when there really isn't) can cause anxiety and is usually followed by more tests (such as biopsy), which also have risks. A biopsy to diagnose lung cancer can cause part of the lung to collapse. Sometimes surgery is needed to reinflate the lung. Harms of diagnostic tests may happen more often in patients who have medical problems caused by heavy or long-term smoking.
Chest x-rays and CT scans expose the chest to radiation.
Radiation exposure from chest x-rays and low-dose CT scans may increase the risk of cancer. Younger people and people at low risk for lung cancer are more likely to develop lung cancer caused by radiation exposure from screening than to be spared death from lung cancer.
Talk to your doctor about your risk for lung cancer and your need for screening tests.
Talk to your doctor or other health care provider about your risk for lung cancer, whether a screening test is right for you, and about the benefits and harms of the screening test. You should take part in the decision about whether a screening test is right for you. For more information, see Cancer Screening Overview.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about lung cancer screening. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Lung Cancer Screening. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lung/patient/lung-screening-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389428]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Updated:
Source URL: https://www.cancer.gov/node/4980/syndication
Source Agency: National Cancer Institute (NCI)
Captured Date: 2013-09-14 09:02:33.0