Feature
Einstein’s Neuroscience Department at 50: Building on a Tradition of Excellence
August 20, 2024
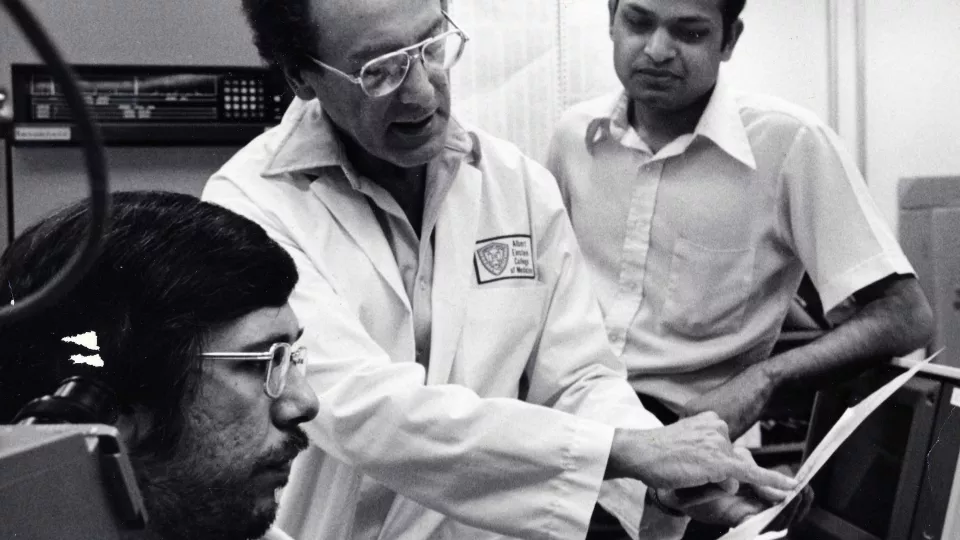
When Einstein’s department of neuroscience was created in 1974, it was one of the first such departments in the country. The term “neuroscience,” in fact, had only recently been coined. The department almost immediately became a mecca for promising young scientists, many attracted by the opportunity to be mentored by distinguished faculty members.
“Those early years were a fantastic and vibrant time, with an enormous amount of electrophysiology research and pioneering work on Alzheimer’s and intellectual disabilities,” said Emeritus Professor Steven Walkley, D.V.M., Ph.D., a department member from 1978 (when he came to Einstein as a graduate student in Dr. Purpura’s lab) until his retirement in January.
Over the decades, leaders in the field have called Einstein home: the founding chair and namesake of the department, Dominick P. Purpura, M.D., Michael Bennett, Ph.D., Peter Davies, Ph.D., Isabelle Rapin, M.D., and Scott Emmons, Ph.D., to name a few.
Fifty years after its creation, the Dominick P. Purpura Department of Neuroscience is now home to 100 scientists—50 active faculty members, 25 postdocs and staff scientists, and 50 graduate students—who are extending the department’s reputation for innovative and groundbreaking research into the next half century.
“Einstein has always attracted researchers who are deeply curious about brain function and are driven to uncover the mechanisms that maintain healthy brain behavior or, when dysfunctional, lead to disease,” said Adam Kohn, Ph.D., interim chair of the department and professor of ophthalmology & visual science and systems & computational biology. “And our current faculty is continuing the outstanding research that the department is known for.”
Einstein neuroscientists are pursuing research in many different areas, including learning and memory; the role of glial cells in brain function; the neural basis of decision making and drug addiction; sensory processing; neurodevelopment; the pathophysiology of eating disorders; synaptic plasticity; and the molecular underpinnings of social behavior. Below we describe the work of four of them.
Pablo Castillo, M.D., Ph.D.
Sussing Out Synapses
As a young doctor, Pablo Castillo, M.D., Ph.D., intended to specialize in neurology and psychiatry. “But I soon grew frustrated by how little we knew about how the brain works and how to effectively treat people with brain disorders,” he said. “Slowly but surely, I followed my interests into the research side of things.”
At the time, universities in his native Uruguay didn’t offer a Ph.D. program, so he moved to the U.S. to study how brain cells communicate. Some thirty years later, Dr. Castillo is the Harold and Muriel Block Chair of Neuroscience at Einstein and a professor in the Dominick P. Purpura Department of Neuroscience and of Psychiatry and Behavioral Sciences. He is still working to better understand how neurons (nerve cells) talk to one another.
“Those connections between neurons,” he points out, “govern absolutely everything—how we think, feel, act, and learn.”
Neurons communicate with each other at the junctions between them called synapses, which, Dr. Castillo explains, work like valves in a water pipe to control the flow of information. His lab studies synaptic plasticity: how molecular and cellular processes change the strength of the connections between neurons based on brain activity that occurs, for example, when you memorize or experience something. Many brain disorders involve dysfunctional neural connections, and Dr. Castillo’s goal is to understand why they go awry.
When Dr. Castillo started his research career, neuroscience was focused on how neuronal activity during learning modifies excitatory synapses, with a pre-synaptic neuron releasing a neurotransmitter to excite a post-synaptic neuron. His lab was among the first to study how neuronal activity modifies inhibitory synapses, in which a pre-synaptic neuron releases a neurotransmitter to suppress the activity of the post-synaptic neuron, thereby reducing the information flow.
Moreover, his group found that long-lasting changes in inhibitory synaptic transmission could be mediated by endogenous cannabinoids (i.e., those made by the body) that are released by neuronal activity. “That immediately opened up many possibilities for looking at other synapses in multiple brain structures,” he said. “What we discovered some two decades ago is part of a more general principle that neural connections are more complicated than we initially realized.”
Dr. Castillo’s research into neural communication has shed light on mechanisms underlying several neurological disorders. For example, in a 2022 study published in the Proceedings of the National Academy of Sciences, he and colleagues describe how epileptic seizures initiate a positive feedback loop in the brain that, in turn, triggers more seizures. “Once you know how that brain circuit operates, you can target treatments to interrupt that positive feedback loop before it causes permanent brain damage,” he said.
Dr. Castillo also studies synaptic proteins: the several types of proteins that play key roles in determining the structure and function of synapses—and, when dysfunctional, can cause problems including autism spectrum disorder, intellectual disability, depression, and schizophrenia. In another 2022 study published in the journal Neuron, he and colleagues found that the protein responsible for Fragile X Syndrome, the most common cause of intellectual disability, regulates protein synthesis within the presynaptic boutons (the “end feet” of axons) from which neurotransmitters are released. Dysregulated neurotransmitter release may therefore contribute to the brain dysfunction observed in Fragile X Syndrome.
“The revolution on the horizon in neuroscience is to be able to elucidate the causal mechanisms of brain diseases well enough to target them with specific therapies,” Dr. Castillo said. “We’re making progress against diseases such as Alzheimer’s, schizophrenia, and autism spectrum disorders. I predict that within a few decades, we’ll know so much more about brain function and connectivity that we will be able to intervene and treat them in much more effective ways.”
Jelena Radulovic, M.D., Ph.D.
Trauma Can Help Make Memories
Jelena Radulovic, M.D., Ph.D., is fascinated by memory and how stress affects it. “Why do some people go through a traumatic event and can move past it while others constantly relive it?,” she asks. “How can our brains store these memories in a way where we are not even conscious of them, yet they still affect our behavior?”
Research has shown that stress-related memories are very different from other memories. “My lab is interested in exploring why this is, with the ultimate goal of seeing if we can modulate the adverse emotional effects of memories involving stress.”
Specifically, she is investigating the molecular mechanisms by which memories of stressful events cause brain dysfunctions in mice similar to those found in people: fear, anxiety, depression, and posttraumatic stress disorder (PTSD). She wants to identify novel therapies that can alleviate or even cure these stress-related psychiatric problems.
Another area of focus is the role of inflammation in forming memories. Inflammation and DNA damage in brain neurons are usually best avoided, since they can lead to neurological problems such as Alzheimer’s and Parkinson’s disease. But in the right place, these “deleterious” changes can create the conditions needed to form long-lasting memories.
Dr. Radulovic, professor in the Dominick P. Purpura Department of Neuroscience, professor of psychiatry and behavioral sciences, and the Sylvia and Robert S. Olnick Chair in Neuroscience at Einstein, reported these findings in March in the journal Nature.
The hippocampus has long been known as the brain’s memory center. Memories were thought to form when a novel stimulus triggers rapid gene expression in clusters of hippocampal neurons. However, the resultant changes seemed to be transient and didn’t explain the formation of a long-term memory.
Dr. Radulovic suspected that another mechanism in the hippocampus must be involved in memory making. In experiments involving mice, she and her colleagues found that long-term memories form when stimuli elicit a pulse of electricity strong enough to damage the DNA in certain hippocampal neurons. What follows is an inflammatory response that—in repairing the DNA damage—etches the memory into the neurons.
“We observed strong activation of genes involved in the Toll-Like Receptor 9 (TLR9) pathway,” said Dr. Radulovic. “This inflammatory pathway is best known for triggering immune responses by detecting small fragments of pathogen DNA,” said Dr. Radulovic, who is also director of the Psychiatry Research Institute at Montefiore Einstein (PRIME). “So, at first, we assumed the TLR9 pathway was activated because the mice had an infection. But looking more closely, we found, to our surprise, that TLR9 was activated only in clusters of hippocampal cells that showed DNA damage.”
During the week required to complete the inflammatory process, the mouse memory-encoding neurons were found to have changed in various ways, including becoming more resistant to new or similar environmental stimuli. “This is noteworthy,” said Dr. Radulovic, “because we’re constantly flooded by information, and the neurons that encode memories need to preserve the information they’ve already acquired and not be ‘distracted’ by new inputs.”
Dr. Radulovic said her findings suggest an interesting possibility. “It could be that Alzheimer’s and other neurodegenerative diseases occur when the DNA damage-and-repair cycle for encoding long-term memories breaks down, causing mutations to accumulate in neuronal DNA,” she said.
Renata Batista-Brito, Ph.D.
The Wonders of Brain Development
“As the mother of three little kids, I’m constantly amazed to see them reach their developmental milestones,” said Renata Batista-Brito, Ph.D. “One moment they’re crawling, the next they’re wobbling on two legs, and before you know it, they’re running to and from.”
Most parents are left to wonder how this happens. But for Dr. Batista-Brito, a neuroscientist, understanding the biology behind these developmental miracles is part and parcel of her day job. She is particularly interested in a less-studied class of brain cells called inhibitory neurons (INs). Quite small in number, INs have an outsize influence on development and on the function of the cortex—the outer most brain layer, which integrates cognitive information such as perception, memory, language, and behavior.
Over the decades, excitatory neurons—which propagate electrical signals throughout the brain—have monopolized researchers’ attention. “But if all you had were excitatory neurons, your brain would be continually seizing up due to overexcitation,” said Dr. Batista-Brito. “INs prevent that from happening by controlling the ways and the speed at which signals get processed in the cortex. If excitatory neurons are the roadways that convey information, INs are the traffic lights that keep everything in check.”
Dr. Batista-Brito started investigating cortical neurons as a graduate student, when she discovered a number of genes that regulate their specificity and development. Based on these mouse studies, she and others found evidence that disruptions of these genes may contribute to various psychiatric disorders in humans.
However, genes tell only part of the story of INs. Now, she’s examining how behavioral states—e.g., sleep, quiet wakefulness, and arousal—affect the activity of these brain cells. “The basic idea is that the way your brain processes information depends on your internal state. If you’re drowsy, how your INs function and what your brain registers are very different than if you’re rested and attentive,” said Dr. Batista-Brito, who is assistant professor in the Dominick P. Purpura Department of Neuroscience and of genetics and of psychiatry and behavioral sciences.
“Development is a remarkable process,” she said. “It has to be well programmed, but it also has to be flexible. There’s a dynamic interplay between one’s genetic programming and one’s experience and environment. The better we can understand this normal interplay, the better we understand what goes wrong in disease and perhaps learn how to correct it.”
Dr. Batista-Brito’s wide-ranging studies are beginning to tease apart the roles of different types of INs in the cortex and determine, for example, how INs: influence the waves of synchronous electrical cortical activity that occur during sleep and at other times; sculpt cortical circuits during development and throughout life; and contribute to reduced visual perception, autism spectrum disorders, and schizophrenia when their activity is disrupted.
INs could be involved in many other diseases as well. “We have not been able to look before,” she said. “But now we have tools to study these cells in animal models and in human patients, allowing us to characterize different disease states. These are such exciting times, and we’re just getting started.”
Peri Kurshan, Ph.D.
Honey Bees, Fruit Flies, and Roundworms, Oh My!
Reading through the scientific papers of Peri Kurshan, Ph.D., is like embarking on a miniature safari. One year she’s working with honey bees, the next with fruit flies or frogs or roundworms. They all have relatively simple and genetically manipulatable nervous systems, allowing a researcher to study how brain neurons work and how their failure leads to a number of neurodevelopmental and neuropsychiatric disorders.
Dr. Kurshan, assistant professor in the Dominick P. Purpura Department of Neuroscience and of genetics, joined the Einstein faculty in 2019. She is particularly interested in the formation and function of synapses, the tiny gaps across which neurons communicate with each other.
“Synapses are the fundamental information processing unit in the brain,” she said. “These connections allow us to store memories, to learn, and to adapt to our environment.” The human brain is thought to contain 100 trillion synapses, and the richness and variety of those connections make each of us who we are.
The goal of one of Dr. Kurshan’s current studies is identifying the initial steps in synapse development. She has found that the accepted origin story of synapses is incomplete. “Proteins called neurexins were thought to initiate synapse formation, but this has never been confirmed in animal studies,” she said.
Using the diminutive roundworm (whose neurons have many equivalents in people), Dr. Kurshan has identified proteins that precede neurexins in synapse formation. Among these is SYD-1, a protein that clusters near the cell membrane to create a scaffold for other synapse-building molecules. Once in place, SYD-1 recruits neurexin proteins, which are cell-adhesion molecules that bring neurons close enough that a synapse can be formed.
“Errors in synapse development are closely associated with a variety of neurodevelopmental and neuropsychiatric disorders including autism spectrum disorders and schizophrenia. In addition, the inappropriate re-activation of processes that normally occur early in development, such as synapse ‘pruning,’ may contribute to Alzheimer’s and other degenerative diseases,” said Dr. Kurshan, whose research is supported by a grant from the National Institutes of Health (NIH). “If we have any hope of ameliorating these disorders, it’s important to know exactly what it is we’re trying to fix.”
In another NIH-funded study, Dr. Kurshan is using the roundworm to understand how mutations in a gene called CACNA1A impair synapses. CACNA1A isinvolved in the transport of calcium ions across cell membranes, a process that contributes to vital cellular functions, including the transmission of signals across synapses.
Dr. Kurshan’s CACNA1A study originated with the “Gene Team” at the Rose F. Kennedy Intellectual and Developmental Disabilities Research Center (IDDRC), which identifies young patients with rare genetic disorders and recruits basic scientists to study how those genetic anomalies cause disease. One such patient came to the IDDRC in 2018 with global developmental disabilities and was found to have mutated CACNA1A. Dr. Kurshan and several other Einstein researchers are studying this gene.
While some patients with CACNA1A mutations experience movement disorders, others have intellectual disabilities. What accounts for these varied clinical presentations, and how to treat them, is a mystery that Dr. Kurshan hopes to solve.