Feature
IDD Gene Team: Breaking Barriers, Empowering Parents, Inspiring Trainees, Advancing Understanding
February 7, 2025
In 2017, the Rose F. Kennedy Intellectual and Developmental Disabilities Research Center (RFK IDDRC) developed a program called IDD Gene Team. Its purpose was to bring together families affected by rare genetic diseases with physicians, basic scientists, and their trainees, so the families could better understand their child’s disorder. At these team meetings, family members share their child’s medical and personal history, physicians describe the broader clinical consequences of the condition, and scientists provide accessible tutorials focused on the fundamental biology of relevant genes. Each year, two or more of these meetings take place, involving a wide range of gene variants causing neurodevelopmental disorders.
The outcomes of team meetings have been overwhelmingly positive, with families not only expressing deep gratitude, but many becoming empowered enough to establish foundations dedicated to their child’s specific condition. Physicians, and in particular the scientists and their trainees, have gained a deeper understanding of the challenges faced by affected families, broadening their perspective on how their research can extend beyond the laboratory. Remarkably, scientists attending these meetings often end up incorporating the patient-specific gene variants into their research. As these studies progress and family-founded organizations expand their efforts, national and international collaborations emerge. Ultimately, the IDD Gene Team program advances understanding and treatment of rare and ultra-rare diseases, benefiting families, physicians, scientists, and the broader medical community.
SIN3A Gene Team
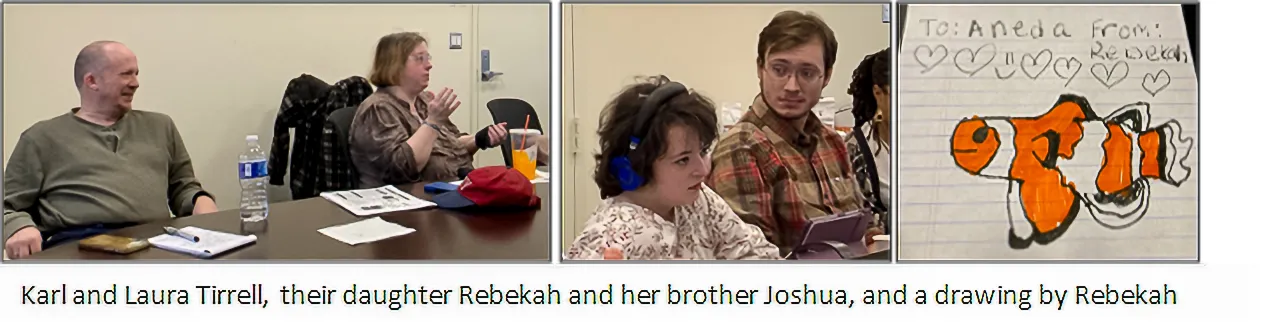
The IDDRC leadership sponsored two IDD Gene Team meetings in 2024. The first, hosted by Dr. Steven Walkley, was held on February 1 in the Kennedy Center. Participants included the Tirrell family which includes parents Laura and Karl, their 18-year-old daughter Rebekah, recently diagnosed with Witteveen-Kolk syndrome due to a SIN3A variant, and her older brother Joshua. Robert Marion, M.D., PhD. served as the host clinician, with Anita Autry, PhD as the presenting scientist. Seven trainees from Einstein laboratories also attended, including three postdoctoral fellows (Carlos Rivero-Quiles, PhD, Annie Maguire, PhD, and Tushar Arora, PhD), three graduate students (Sarah Goebel, Dylann Cordova Martinez, and Victoria Sedwick), and one medical student (Madeline Klein).
The meeting began with family introductions, during which Laura and Karl shared Rebekah’s medical journey, including developmental delays, seizures, immunological issues, and scoliosis. Rebekah described her experiences growing up, including a recent difficult scoliosis surgery, with Joshua offering additional perspectives. The students and postdocs engaged the family with thoughtful questions. Dr. Marion then provided further clinical context about Rebekah’s early years and Witteveen-Kolk syndrome. This was followed by Dr. Autry describing how SIN3A encodes a multi-functional protein regulating gene expression during fetal development, which accounts for the diverse features of this complex syndrome. She noted that while model systems are being developed, much remains to be learned about this complex gene. Interestingly, while Rebekah listened attentively, she was also busy drawing a picture which she presented to Dr. “Aneda,” a heartfelt gesture that concluded the meeting on a warm note.
IRF2BPL Gene Team
The second meeting in 2024 focused on variants in the gene IRF2BPL, which cause a condition known as NEDAMSS (Neurodevelopmental Disorder with Regression, Abnormal Movements, Loss of Speech, and Seizures). Uniquely, it brought together two families —Chris and Angela Papazoglou with their 4-year-old son Yiannis, and Maria and Sandy Rodriguez with their 16-year-old son Berny—who had never met before.The meeting was hosted by Steven Walkley, PhD with other faculty attending including Dr. Sophie Molholm and Bryen Jordan, PhD. Dr. Jordan served as a translator for Mr. Rodriguez whose English was limited. Also attending were Berny’s physician Melissa Wasserstein, M.D., genetic counselor Monisha Sebastian, and Einstein scientists, Richard Stanley, Ph.D., and Violeta Chitu, Ph.D. Trainees attending included postdoctoral fellow Carlos Rivero-Quiles, graduate students Sarah Goebel and Dylann Cordova Martinez, and medical student Madeline Klein. The session was filmed by Einstein’s director of multimedia communications, Sunita Reed and members of her film crew.
The meeting opened with introductions before Maria Rodriguez shared the powerful story of her son Berny. From an early age, Berny faced delays in walking and talking, and at 11, suffered his first seizure. As he entered his teens, his language and motor skills began to regress. By his 20s, Berny was wheelchair-bound and non-verbal. Genetic testing revealed a spontaneous genetic variant in IRF2BPL, which provided some answers about his condition. Angela Papazoglou then shared the journey of her 4-year old son, Yiannis, who was diagnosed with a variant in the same gene. For both families, this meeting marked the first time they had connected with others facing the same rare diagnosis. The emotional exchange between them highlighted the isolation that often accompanies ultra-rare diseases.
Dr. Wasserstein then provided additional clinical context. She explained that individuals with pathogenic variants in IRFBPL2 typically experience early neurodevelopmental delays, seizures, and a progressive decline in function during the first two decades of life. Dr. Chitu followed with a lay summary of the role of this gene in cellular function. She noted that although the gene is widely expressed throughout the body, the brain is especially vulnerable to its loss. On a promising note, she explained that part of the neuronal dysfunction is linked to overactive mitochondrial function in astrocytes and that recent studies have identified a potential drug that might help alleviate this aspect of the disease. Drs. Chitu and Stanley stressed the urgent need to develop a mouse model to study this disease and test this therapy- a critical step toward potential treatment.
Two significant outcomes emerged from this meeting: The first is that the efforts of Sunita Reed and the Einstein communications department led to a video available for viewing.
The second is that the research project to develop a mouse model to investigate this disease has been funded by an RFK IDDRC Pilot Research Grant.