Feature
Recipes for Retinas
June 7, 2024
Wei Liu, Ph.D., studies the retina and is an expert in developing retinal organoids, mini-retinas grown from human pluripotent stem cells. When the National Eye Institute (NEI), a part of the National Institutes of Health, launched a competition for developing a three-dimensional retinal organoid, only Dr. Liu succeeded in winning all three stages of the challenge.
“Wei is an innovative scientist whose research is leading toward the development of functional human eyes in a dish,” said Roy Chuck, M.D., Ph.D., the Paul Henkind Chair of Ophthalmology & Visual Sciences at Einstein and Montefiore. “His advances may make it possible to use lab-grown tissue to replace diseased or damaged retinas—an achievement with the potential for helping millions of people worldwide.”
A native of Tianjin, China, Dr. Liu earned his Ph.D. in molecular biology at the Institute of Biophysics of the Chinese Academy of Sciences and then completed a postdoctoral fellowship at St. Jude Children’s Research Hospital in Memphis, TN. He joined the Einstein faculty in 2010, where he is an associate professor of ophthalmology and visual sciences and of genetics.
Why did you choose to study the retina?
The retina fascinated me because its biology is an exciting area for basic research and it's also so clinically significant for healthy vision. I’m particularly interested in how the retina develops in the embryo and how defects in its development lead to inherited retinal diseases. Since the retina is a part of the central nervous system, a better understanding of the retina helps decipher the biology of the brain.
What do you consider your first major scientific finding?
My early studies revealed the important role of a gene called Six3 in the embryonic development of the forebrain and of the lens and retina of the eye. Mutations in this gene cause drastic defects in the forebrain and in eye development.
Did your Six3 studies involve animal models?
Yes, to learn about Six3’s function, I studied mice in which the Six3 gene was knocked out.
Do mouse embryos resemble human embryos?
Yes, early development of the forebrain and eye is very similar in the two species.
What are the limitations of using mice to study the retina?
The most important one is that the mouse retina lacks the macular and fovea— anatomical features unique to the mature retina of humans and other primates. The macula is the small but important part of the retina that translates the light that enters your eyes into electrical signals for visual information processing. The fovea, a tiny depression within the macula, is especially rich in cones, which enable us to see color and fine details. [See illustration]. Due to this anatomical difference, mouse models aren’t often useful for studying macular diseases such as age-related macular degeneration. Other mouse-human differences pertain to cell types and gene expression.
Is that why you’ve added organoids to your studies?
Yes. Retinal organoids are derived from human pluripotent stem cells, so they mimic the human retina in structure, cell types, and gene expression during development. As our research has progressed, this resemblance continues to improve. Such organoid models are profoundly changing studies of the human retina.
You’ve written that your organoid-making methods are efficient and scalable. What does that mean?
That means we can now generate retinal organoids with fewer manual manipulations, in much greater numbers—thousands at a time, which makes them more cost-effective than earlier versions.
You’re the only scientist to win prizes in all three National Eye Institute 3-D retinal organoid challenges, in 2018, 2020, and 2022. What did these awards recognize?
Over that time span, we’ve developed two new and different types of organoids that advance the ability to replicate and study the human retina in the laboratory.
I’m hopeful that our work with retinal organoids will soon make it possible for tissue transplants to help in treating retinal diseases.
Wei Liu, Ph.D.
Could you describe the two organoids and how you’re using them?
One type is a three-dimensional cone-rich retinal organoid. We’re using it to study two things: the mechanisms of retinal differentiation, and the inherited retinal diseases caused by recessive mutations in the gene CRB1; those diseases include retinitis pigmentosa 12 and Leber Congenital Amaurosis 8. We want to determine the function of CRB1 in human retinal tissues and how CRB1 mutations cause retinal diseases.
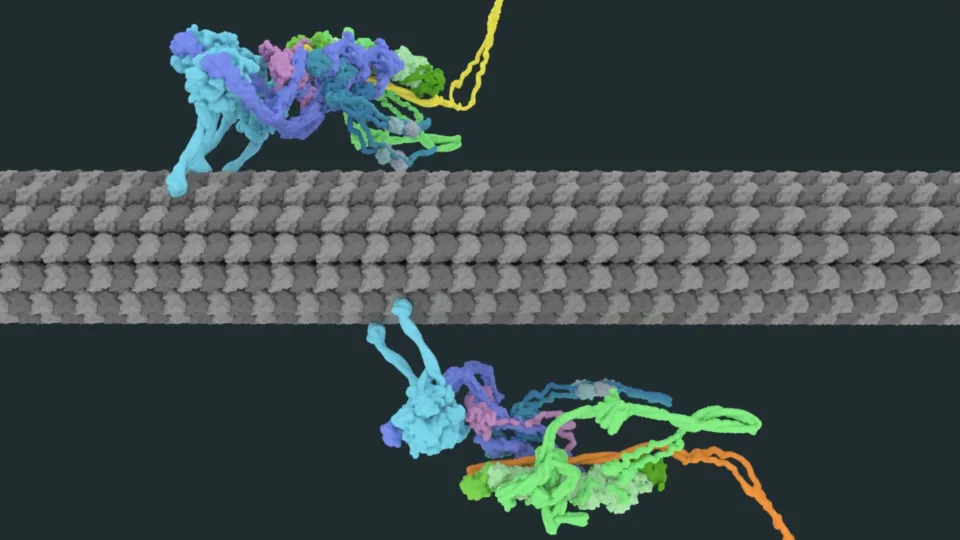
We call the second type of organoid the CONCEPT telencephalon-eye organoid. It contains the telencephalon [i.e., the cerebral hemispheres] and ocular tissues including the optic stalk, optic disc, and neural retina. The acronym CONCEPT stands for concentric zones of anterior ectodermal progenitors. What’s exciting about CONCEPT is that it’s the first retinal organoid that possesses optic disc and stalk tissues, which—in human fetal retinas and in our CONCEPT retinal organoid—provide axon growth and pathfinding cues for retinal ganglion cells (RGCs).
It’s the degeneration of RGCs and their axons that leads to glaucoma and other optic nerve diseases. Now that we’ve developed a one-step method for isolating RGCs from human organoids via a cell surface biomarker identified in our study, we can test drugs that might be able to protect RGCs and also explore cell replacement therapies for treating RGC-related diseases such as glaucoma.
Could organoids be used to generate RGCs and other retina cells for transplantation?
Several laboratories are evaluating the therapeutic benefit of transplanting organoid-derived retinal cells. To restore vision, transplanted cells must integrate into the host retina and form proper connections with the existing visual system, which has not yet been convincingly demonstrated. But I’m hopeful that our work with retinal organoids will soon make it possible for tissue transplants to help in treating retinal diseases.